Evolution of Eustachian Tube Surgery: 300 Years and Counting
Edward D. McCoul, MD, MPH Physicians have sought an effective treatment for dysfunction of the Eustachian tube (ET) for nearly three centuries. The earliest recorded attempts from the early 18th century involved transoral or transnasal catheterization, though which insufflation and irrigation with various substances could be applied. Forcible bougie dilation and endoluminal irradiation are described in several historical sources. The practice of catheterization continued through the 19th century, while very few surgeons attempted surgical reconstruction of the ET. Until the late 20th century, the prevailing belief among surgeons and anatomists was that the ET is a passive conduit with a relatively static lumen. Most surgeons presumed that ET dysfunction was caused by a stenosis in the bony portion of the ET; techniques for drilling the temporal bone were described for both the transcanal and middle fossa approaches. Subsequent attempts to improve middle ear aeration sought to bypass the ET entirely. Tympanomaxillary shunting, tympanofrontal shunting, and transposition of Wharton’s duct were all described with limited acceptance. Each of these techniques was aimed at relieving obstruction at the ET isthmus within the temporal bone. The later 20th century brought a paradigm shift in which the ET was viewed not as a static structure but a dynamic one. The availability of fiberoptic endoscopy facilitated observation of a valve-like function of the cartilaginous ET; abnormal closure of this valve is now believed to underlie most cases of ET dysfunction. Misurya reported in 1976 on the “functional Eustachian tuboplasty,” wherein the action of the tensor veli palatini was augmented by lessening the length of its tendon. Jansen described in 1985 a mucosal-sparing technique to resect the posterior portion of the ET. A handful of other techniques received little lasting attention. The most recent wave of innovations in ET surgery has been marked by the adaptation of current rhinologic techniques. In 1997, Kujawski introduced the laser Eustachian tuboplasty, whereby mucosa and cartilage were obliterated from the posterior wall of the ET. Metson et al subsequently reported on a transnasal endoscopic technique that entailed removal of mucosa from the torus tubarius using a tissue shaver. Modifications of the laser tuboplasty have also been described. Current interest in ET surgery focuses on the cartilaginous portion of the ET as the site of pathology in ET dysfunction. The newest technique involves endoscopic-guided balloon catheter dilation, which builds upon previous efforts that have established the ET as a dynamic organ. Ongoing studies of the ideal intervention for ET dysfunction are likely to shape the treatment of this disorder in years to come. Dr. McCoul’s article is based on the paper presented at the Otolaryngology Historical Society meeting, September 12, 2011. If you are interested in presenting at the 2012 OHS meeting, September 10, in Washington, DC, or wish to join or renew as an OHS member, contact museum@entnet.org.
Edward D. McCoul, MD, MPH
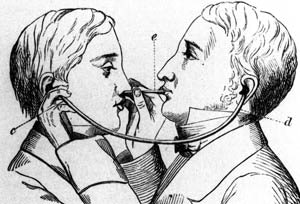 Eustachian tube catheterization with a diagnostic tube in use. From Kramer’s Aural Surgery of the Present Day (1863).
Eustachian tube catheterization with a diagnostic tube in use. From Kramer’s Aural Surgery of the Present Day (1863).Physicians have sought an effective treatment for dysfunction of the Eustachian tube (ET) for nearly three centuries. The earliest recorded attempts from the early 18th century involved transoral or transnasal catheterization, though which insufflation and irrigation with various substances could be applied. Forcible bougie dilation and endoluminal irradiation are described in several historical sources. The practice of catheterization continued through the 19th century, while very few surgeons attempted surgical reconstruction of the ET.
Until the late 20th century, the prevailing belief among surgeons and anatomists was that the ET is a passive conduit with a relatively static lumen. Most surgeons presumed that ET dysfunction was caused by a stenosis in the bony portion of the ET; techniques for drilling the temporal bone were described for both the transcanal and middle fossa approaches. Subsequent attempts to improve middle ear aeration sought to bypass the ET entirely. Tympanomaxillary shunting, tympanofrontal shunting, and transposition of Wharton’s duct were all described with limited acceptance. Each of these techniques was aimed at relieving obstruction at the ET isthmus within the temporal bone.
The later 20th century brought a paradigm shift in which the ET was viewed not as a static structure but a dynamic one. The availability of fiberoptic endoscopy facilitated observation of a valve-like function of the cartilaginous ET; abnormal closure of this valve is now believed to underlie most cases of ET dysfunction. Misurya reported in 1976 on the “functional Eustachian tuboplasty,” wherein the action of the tensor veli palatini was augmented by lessening the length of its tendon. Jansen described in 1985 a mucosal-sparing technique to resect the posterior portion of the ET. A handful of other techniques received little lasting attention.
The most recent wave of innovations in ET surgery has been marked by the adaptation of current rhinologic techniques. In 1997, Kujawski introduced the laser Eustachian tuboplasty, whereby mucosa and cartilage were obliterated from the posterior wall of the ET. Metson et al subsequently reported on a transnasal endoscopic technique that entailed removal of mucosa from the torus tubarius using a tissue shaver. Modifications of the laser tuboplasty have also been described.
Current interest in ET surgery focuses on the cartilaginous portion of the ET as the site of pathology in ET dysfunction. The newest technique involves endoscopic-guided balloon catheter dilation, which builds upon previous efforts that have established the ET as a dynamic organ. Ongoing studies of the ideal intervention for ET dysfunction are likely to shape the treatment of this disorder in years to come.