SGR Repeal Gains Momentum in U.S. House of Representatives
The Sustainable Growth Rate (SGR) formula, the flawed mechanism used to calculate payments to physicians within the Medicare program, has been the proverbial “thorn-in-the-foot” issue for the physician community for more than a decade. Created by the Balanced Budget Act of 1997, the SGR formula was intended to control growth in Medicare payments for physician services by basing payments on per capita growth in the gross domestic product (GDP). Under the SGR formula, physician payments are reduced when growth in Medicare patients’ use of physician services exceeds the universal spending target set by the SGR formula. By faulty design, a weak economy could trigger a decrease in target spending even if use of physician services remained high. As a result, physicians have annually faced steep cuts to their payment rate, forcing Congress to take action almost every year to avert massive cuts in the Medicare system. Since the trend toward negative annual payment updates began, the AAO-HNS and others in the physician community have continually urged Congress to repeal the flawed formula and replace it with a payment framework that would provide stability for physicians practicing within the Medicare program and ensure critical access to care for the nation’s senior population. In this case, however, Congress’ annual actions to avert the payment cuts have acted as a double-edged sword. The good? Steep payment cuts for physicians have been avoided. The bad? In most cases, Congress failed to identify appropriate “pay fors” to fund the elimination of each year’s scheduled cuts. As a result, the Congressional Budget Office (CBO) estimated the cumulative debt associated with the SGR had grown to more than $300 billion by the end of 2012. Despite wide conceptual support by both Democrats and Republicans for repealing the flawed SGR formula, the immense cost associated with such action has proved prohibitive. However, based on early Congressional attention and an updated cost analysis by CBO, it seems 2013 may be the year that the stars align and Congress finally takes action to fully repeal the SGR formula. A Rare Opportunity The first piece of good news for this year came in the form of a Congressional hearing. In February, the Health Subcommittee of the House Energy and Commerce Committee gathered to discuss and evaluate key components for developing a new Medicare physician payment model. While hearings on this topic are not particularly out of the ordinary, its scheduling so early in the 113th Congress signaled that SGR reform was a front-burner issue for many Members of Congress. Soon thereafter, staff from the House Ways and Means Committee invited various physician specialty groups, including the AAO-HNS, to participate in a briefing session on the Committee’s development of a proposal to repeal the SGR and put in place a framework for a Medicare physician payment system designed to incentivize the delivery of efficient, high-quality healthcare. During the meeting, Committee staff emphasized their need for input from the physician community and made a request for official written comments from all the groups in attendance. Given the rare opportunity to take part in the infancy stages of developing a potential new payment model, the AAO-HNS Government Affairs and Health Policy teams, in conjunction with the Academy’s Physician Payment Policy (3P) and Ad Hoc Payment Workgroup, began drafting comments specific to otolaryngology-head and neck surgery. In the past, most legislative proposals regarding the SGR have attempted to move the Medicare physician payment system to a one-size-fits-all approach. However, this year’s initial proposal shows that Members of Congress have begun to understand that, given the dynamic nature of modern healthcare delivery, any payment model must also provide options to accommodate providers across the continuum of care. The AAO-HNS has emphasized that in any sort of payment mechanism, each specialty must be afforded the opportunity to drive the metrics and/or standards by which they are measured. Given the complexity of developing a new payment system and the time required to adapt and test the functionality of new programs, the AAO-HNS also underscored the need for providing a stable payment period for all physicians within the Medicare program following the initial repeal of the SGR. The Academy’s official comments, dated February 26, 2013, are available at www.entnet.org/advocacy. While no one will argue about Washington’s love of a wonky policy scheme, even the best intended proposal could become moot if costs remain prohibitive, right? Here lies the last bit of encouraging news regarding the possibility of SGR repeal in 2013. Also in February, the CBO announced a massive reduction (to $138 billion) in the estimated cost of repealing the SGR. Following the announcement, a seemingly dead-end issue has been revived in earnest and the chairs of the House Ways and Means and Energy and Commerce Committees have heralded SGR repeal as one of their top priorities. Although no hard timeline had been established at the writing of this article, several Members of Congress are urging leaders to address the SGR issue prior to the August recess. However, it must also be said that despite all of this year’s positive activity, ongoing negotiations to reach a compromise regarding an overall deficit reduction plan pose a serious risk of derailing efforts to address the SGR and many other legislative issues. Nevertheless, the AAO-HNS remains hopeful that 2013 marks the year that the infamous SGR is finally laid to rest. And as many agree, repeal of the SGR is now on sale and Congress should act fast before the CBO changes its mind. For more information about AAO-HNS legislative priorities in the 113th Congress, email legfederal@entnet.org.
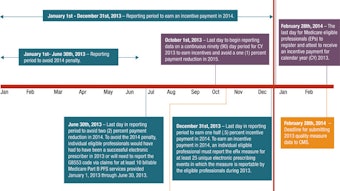
The Sustainable Growth Rate (SGR) formula, the flawed mechanism used to calculate payments to physicians within the Medicare program, has been the proverbial “thorn-in-the-foot” issue for the physician community for more than a decade. Created by the Balanced Budget Act of 1997, the SGR formula was intended to control growth in Medicare payments for physician services by basing payments on per capita growth in the gross domestic product (GDP). Under the SGR formula, physician payments are reduced when growth in Medicare patients’ use of physician services exceeds the universal spending target set by the SGR formula. By faulty design, a weak economy could trigger a decrease in target spending even if use of physician services remained high. As a result, physicians have annually faced steep cuts to their payment rate, forcing Congress to take action almost every year to avert massive cuts in the Medicare system.
Since the trend toward negative annual payment updates began, the AAO-HNS and others in the physician community have continually urged Congress to repeal the flawed formula and replace it with a payment framework that would provide stability for physicians practicing within the Medicare program and ensure critical access to care for the nation’s senior population. In this case, however, Congress’ annual actions to avert the payment cuts have acted as a double-edged sword. The good? Steep payment cuts for physicians have been avoided. The bad? In most cases, Congress failed to identify appropriate “pay fors” to fund the elimination of each year’s scheduled cuts. As a result, the Congressional Budget Office (CBO) estimated the cumulative debt associated with the SGR had grown to more than $300 billion by the end of 2012.
Despite wide conceptual support by both Democrats and Republicans for repealing the flawed SGR formula, the immense cost associated with such action has proved prohibitive. However, based on early Congressional attention and an updated cost analysis by CBO, it seems 2013 may be the year that the stars align and Congress finally takes action to fully repeal the SGR formula.
A Rare Opportunity
The first piece of good news for this year came in the form of a Congressional hearing. In February, the Health Subcommittee of the House Energy and Commerce Committee gathered to discuss and evaluate key components for developing a new Medicare physician payment model. While hearings on this topic are not particularly out of the ordinary, its scheduling so early in the 113th Congress signaled that SGR reform was a front-burner issue for many Members of Congress.
Soon thereafter, staff from the House Ways and Means Committee invited various physician specialty groups, including the AAO-HNS, to participate in a briefing session on the Committee’s development of a proposal to repeal the SGR and put in place a framework for a Medicare physician payment system designed to incentivize the delivery of efficient, high-quality healthcare. During the meeting, Committee staff emphasized their need for input from the physician community and made a request for official written comments from all the groups in attendance.
Given the rare opportunity to take part in the infancy stages of developing a potential new payment model, the AAO-HNS Government Affairs and Health Policy teams, in conjunction with the Academy’s Physician Payment Policy (3P) and Ad Hoc Payment Workgroup, began drafting comments specific to otolaryngology-head and neck surgery. In the past, most legislative proposals regarding the SGR have attempted to move the Medicare physician payment system to a one-size-fits-all approach. However, this year’s initial proposal shows that Members of Congress have begun to understand that, given the dynamic nature of modern healthcare delivery, any payment model must also provide options to accommodate providers across the continuum of care.
The AAO-HNS has emphasized that in any sort of payment mechanism, each specialty must be afforded the opportunity to drive the metrics and/or standards by which they are measured. Given the complexity of developing a new payment system and the time required to adapt and test the functionality of new programs, the AAO-HNS also underscored the need for providing a stable payment period for all physicians within the Medicare program following the initial repeal of the SGR. The Academy’s official comments, dated February 26, 2013, are available at www.entnet.org/advocacy.
While no one will argue about Washington’s love of a wonky policy scheme, even the best intended proposal could become moot if costs remain prohibitive, right? Here lies the last bit of encouraging news regarding the possibility of SGR repeal in 2013. Also in February, the CBO announced a massive reduction (to $138 billion) in the estimated cost of repealing the SGR. Following the announcement, a seemingly dead-end issue has been revived in earnest and the chairs of the House Ways and Means and Energy and Commerce Committees have heralded SGR repeal as one of their top priorities.
Although no hard timeline had been established at the writing of this article, several Members of Congress are urging leaders to address the SGR issue prior to the August recess. However, it must also be said that despite all of this year’s positive activity, ongoing negotiations to reach a compromise regarding an overall deficit reduction plan pose a serious risk of derailing efforts to address the SGR and many other legislative issues.
Nevertheless, the AAO-HNS remains hopeful that 2013 marks the year that the infamous SGR is finally laid to rest. And as many agree, repeal of the SGR is now on sale and Congress should act fast before the CBO changes its mind.
For more information about AAO-HNS legislative priorities in the 113th Congress, email legfederal@entnet.org.