The Transition to ICD-10: Will You Be Ready?
Robert R. Lorenz, MD Lee D. Eisenberg, MD After years of delay, the Centers for Medicare & Medicaid Services (CMS) has reiterated that on October 1, 2014, the ICD-9 code sets used to report medical diagnoses and inpatient procedures will be replaced by ICD-10 code sets. This means providers should be preparing now to meet the 2014 deadline for transition. The change does not affect CPT coding for physician services or outpatient procedures. Why ICD-10? The rationale for the transition is based on the fact that ICD-9 cannot be expanded to encompass necessary changes as it has only five numeric characters, whereas ICD-10 will have seven alphanumeric characters. Not only will the total number of diagnostic codes (ICD-10 clinical modification [CM]) be expanded from the current 14,000 to 68,000 codes, but the methodology of coding will be altered, too. This mandated change will have a major effect on documentation and billing in the office and hospital. ICD-9 dates back to 1977, and many changes have occurred in technology and disease processes that are not reflected in the current code set. Due to the lack of detail and specificity in the current ICD-9 code sets, significantly different disease processes are being referred to by a single code, making it difficult to capture detailed diagnostic information and the specificity for accurate billing and reimbursement, especially as it relates to severity and complexity. As members are aware, one of CMS’ primary goals in recent years has been to improve quality of care. Therefore, the lack of precision within the ICD-9 code set, which does not allow for the accurate measurement of quality, has been identified as an area requiring improvement by the agency. Further, since most developed countries converted to ICD-10 in the 1990s, international benchmarking of disease outside the U.S. will be facilitated by our domestic implementation of the ICD-10 code set. In addition to the ICD-10-CM coding system changes, the transition to ICD-10-procedural coding system (PCS) will occur concurrently, but applies only to inpatient procedural coding and will largely affect facility-based coders. Physicians will be largely unaffected by ICD-10-PCS changes and will continue to use the CPT coding methodology to report their medical services. Where Do I Stand? When one examines the scope of changes that the ICD-9 to ICD-10 transformation entails, it is easy to become overwhelmed considering the effects on payers, suppliers, clearinghouses, administrators, schedulers, databases, quality measures, and research registries. By starting with your daily workflow as a physician, your focus should be concentrated on two areas: documentation and provider-based coding. Regarding documentation, we can summarize by stating that the increased level of granularity contained within the diagnosis code will continue to need accurate and sufficient documentation to justify the use of that particular code. The use of the diagnostic code should not be the first time an auditor comes into contact with data describing the pathophysiology, but rather, the detail should be contained within the documentation produced by the provider. Therefore, the specificity requirements in your documentation will be predicated on the new, more specific, diagnostic codes you will be entering. More Specific? In regard to provider-based coding, it is easy to state that the new ICD-10 code set will be more “specific,” but many members have asked what that really means. The new code set contains increased granularity around diseases and will include new information such as, but not limited to, the following: Laterality Specific disease pathophysiology Combination codes Common clinical guidance scales and staging Timing of encounters Increased granularity of disease manifestations Alcohol and drug dependence effects of use Increase in injury codes Sequelae What Does This Coding Change Mean for You? The implication to your coding depends on how your practice is structured and what disease sets you commonly see. One place to start is determining whether you’ll be using an electronic medical record (EMR) by October of 2014. Most EMRs are updating their disease-selection technology (pick-list) to conform to ICD-10 requirements. While this may not automatically convert the code from the ICD-9 to the ICD-10 version for existing patients, choosing a new, more specific ICD-10 code using this technology is not much more onerous than today’s practice. Providers who are using paper-based documentation and billing will experience a significantly more difficult conversion to the new coding system, especially if they are using the actual tabular, numerical code, rather than the alphabetic, disease description, as the new numerical system bears little resemblance to the previous methodology. The administrative burden for converting different categories of diseases will vary according to disease. Some codes will map from one ICD-9 code to merely two or three ICD-10 codes while others may map from one ICD-9 code to 12 ICD-10 codes. The most obvious examples of mapping “one-to-many” (in other words, one ICD-9 code being able to be converted to many potential ICD-10 codes) include orthopedics and obstetrics. But even for our standard “382.01: Acute suppurative otitis media with spontaneous rupture of ear drum” ICD-9 code, we will have to include a side and a timing when converting to “H66.014: Acute suppurative otitis media with spontaneous rupture of eardrum, recurrent, right ear” in ICD-10. To assist with the conversion, CMS has developed a tool called General Equivalence Mapping, or GEM, which aids in the conversion from a code in ICD-9 to ICD-10, and is available online. This can be a straightforward, one-to-one conversion, or a more complicated one-to-many mapping. GEMs have been created for both a forward mapping ICD-9 to ICD-10 conversion, or a backward mapping ICD-10 to ICD-9 conversion. What Will This Cost My Practice? Potential costs of the conversion can vary widely, depending on your IT and administrative support. Providers should plan for an initial decrement in their productivity of five percent to 10 percent during coding functions. If your coding is done for you in your office or the hospital, estimates suggest a decrease in coder efficiency of 20 to 50 percent initially, depending on the site. Most large EMR systems have a robust plan for administrating the ICD-10 conversion, but for providers with practice-specific technology, or worse yet, homegrown systems; a full IT overhaul may be required due to the dependencies with systems that interact with the EMR. Training for physicians and staff will be costly and time consuming. The Medical Group Management Association (MGMA) estimates it will cost $84,000 for a three-physician practice to transition to ICD-10 and up to $3 million for large practices. There are multiple educational vendors with prepared materials for your office staff, billers, and us as providers, to review the changes that are specific to your area of expertise. Providers should plan on four to six hours of physician education in order to learn the content. What Steps Should I Be Taking Now? Providers should communicate with their office manager or financial support personnel to ask for a risk assessment of their practice. This should include questions such as: What will your coding process entail when you are utilizing ICD-10? How much additional documentation will be required, if any, to substantiate the use of the more granular code? Do you have preference lists that can be updated ahead of time to mitigate the disruption to your practice? We also recommend that practices contact their payers and ask what type of infrastructure they are creating to assist with the conversion and whether there will be billing implications for the use of generic or unsubstantiated codes. Providers should also ask what percentage of their practice these codes and payers represent, and what they can do ahead of time to decrease revenue disruption. Remember, improving documentation accuracy to levels required for ICD-10 can begin now, even if your coding remains in the ICD-9 system. Other implementation and planning strategies could include the creation of a pilot with your office staff of dual coding to test the systems you’ve put into place or asking a payer to partner with you on a dual coding project ahead of the October 1, 2014, deadline in an effort to work out their own transition complications. Academy Resources for Transition In an ongoing effort to prepare and educate members regarding the looming transition to the use of ICD-10 diagnostic codes, the Academy has developed a series of educational articles and a dedicated webpage on www.entnet.org as resources for members. In addition, we are working toward an ongoing initiative to develop new resources for members, which will be rolled out during the remainder of 2013 and the first half of 2014. A miniseminar will take place at the 2013 Annual Meeting & OTO EXPOSM in Vancouver, Canada, which will include presentations by ICD-10 experts. Currently available Academy ICD-10 resources include: What’s New: http://www.entnet.org/Practice/International-Classification-of-Diseases-ICD.cfm General Information: http://www.entnet.org/Practice/International-Classification-of-Diseases-ICD.cfm ICD-9 to ICD-10 Crosswalk for Top 200 ENT Codes: http://www.entnet.org/Practice/loader.cfm?csModule=security/getfile&PageID=156407 ICD-9 Coding to the highest level of specificity: http://www.entnet.org/practice/resources/upload/Coordinating%20ICD.pdf Previous Academy Bulletin Articles include: Conforming Your Otolaryngology Documentation to ICD-10: http://bulletin.entnet.org/highlight.aspx?id=2904&p=271 ICD-10: What it Means for Your Practice: http://bulletin.entnet.org/highlight.aspx?id=3516&p=310 Preparing for ICD-10: http://bulletin.entnet.org/highlight.aspx?id=3925&p=333 Other materials that may be useful to members seeking additional information include: CMS PowerPoint on ICD 10 Transition: http://www.cms.gov/Medicare/Coding/ICD10/Downloads/CMSICD-10Overview.pdf CMS Implementation Guide: http://www.cms.gov/Medicare/Coding/ICD10/downloads/ICD10SmallandMediumPractices508.pdf CMS Proposed Timelines for Small, Medium, and Large Practices: http://www.cms.gov/medicare/coding/ICD10/Downloads AMA ICD Transition White Papers: http://www.ama-assn.org/ama/no-index/about-ama/icd10-white-paper-confirmation.page AAPC PowerPoint on Transition: http://www.cms.gov/Medicare/Coding/ICD10/Downloads/AAPCICD-10WillChangeEverything.pdf AAPC FAQ: http://www.aapc.com/icd-10/faq.aspx#why Understanding and Preparing for ICD-10: Making the Conversion from ICD-9 to ICD-10 Manageable: http://www.mgma.com/workarea/downloadasset.aspx?id=1368339
Robert R. Lorenz, MD
Lee D. Eisenberg, MD
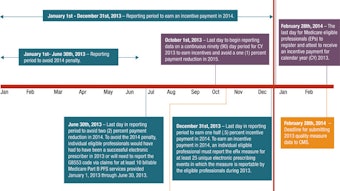
After years of delay, the Centers for Medicare & Medicaid Services (CMS) has reiterated that on October 1, 2014, the ICD-9 code sets used to report medical diagnoses and inpatient procedures will be replaced by ICD-10 code sets. This means providers should be preparing now to meet the 2014 deadline for transition. The change does not affect CPT coding for physician services or outpatient procedures.
Why ICD-10?
The rationale for the transition is based on the fact that ICD-9 cannot be expanded to encompass necessary changes as it has only five numeric characters, whereas ICD-10 will have seven alphanumeric characters. Not only will the total number of diagnostic codes (ICD-10 clinical modification [CM]) be expanded from the current 14,000 to 68,000 codes, but the methodology of coding will be altered, too.
This mandated change will have a major effect on documentation and billing in the office and hospital. ICD-9 dates back to 1977, and many changes have occurred in technology and disease processes that are not reflected in the current code set. Due to the lack of detail and specificity in the current ICD-9 code sets, significantly different disease processes are being referred to by a single code, making it difficult to capture detailed diagnostic information and the specificity for accurate billing and reimbursement, especially as it relates to severity and complexity. As members are aware, one of CMS’ primary goals in recent years has been to improve quality of care. Therefore, the lack of precision within the ICD-9 code set, which does not allow for the accurate measurement of quality, has been identified as an area requiring improvement by the agency. Further, since most developed countries converted to ICD-10 in the 1990s, international benchmarking of disease outside the U.S. will be facilitated by our domestic implementation of the ICD-10 code set.
In addition to the ICD-10-CM coding system changes, the transition to ICD-10-procedural coding system (PCS) will occur concurrently, but applies only to inpatient procedural coding and will largely affect facility-based coders. Physicians will be largely unaffected by ICD-10-PCS changes and will continue to use the CPT coding methodology to report their medical services.
Where Do I Stand?
When one examines the scope of changes that the ICD-9 to ICD-10 transformation entails, it is easy to become overwhelmed considering the effects on payers, suppliers, clearinghouses, administrators, schedulers, databases, quality measures, and research registries. By starting with your daily workflow as a physician, your focus should be concentrated on two areas: documentation and provider-based coding. Regarding documentation, we can summarize by stating that the increased level of granularity contained within the diagnosis code will continue to need accurate and sufficient documentation to justify the use of that particular code. The use of the diagnostic code should not be the first time an auditor comes into contact with data describing the pathophysiology, but rather, the detail should be contained within the documentation produced by the provider. Therefore, the specificity requirements in your documentation will be predicated on the new, more specific, diagnostic codes you will be entering.
More Specific?
In regard to provider-based coding, it is easy to state that the new ICD-10 code set will be more “specific,” but many members have asked what that really means. The new code set contains increased granularity around diseases and will include new information such as, but not limited to, the following:
- Laterality
- Specific disease pathophysiology
- Combination codes
- Common clinical guidance scales and staging
- Timing of encounters
- Increased granularity of disease manifestations
- Alcohol and drug dependence effects of use
- Increase in injury codes
- Sequelae
What Does This Coding Change Mean for You?
The implication to your coding depends on how your practice is structured and what disease sets you commonly see. One place to start is determining whether you’ll be using an electronic medical record (EMR) by October of 2014. Most EMRs are updating their disease-selection technology (pick-list) to conform to ICD-10 requirements. While this may not automatically convert the code from the ICD-9 to the ICD-10 version for existing patients, choosing a new, more specific ICD-10 code using this technology is not much more onerous than today’s practice.
Providers who are using paper-based documentation and billing will experience a significantly more difficult conversion to the new coding system, especially if they are using the actual tabular, numerical code, rather than the alphabetic, disease description, as the new numerical system bears little resemblance to the previous methodology. The administrative burden for converting different categories of diseases will vary according to disease. Some codes will map from one ICD-9 code to merely two or three ICD-10 codes while others may map from one ICD-9 code to 12 ICD-10 codes. The most obvious examples of mapping “one-to-many” (in other words, one ICD-9 code being able to be converted to many potential ICD-10 codes) include orthopedics and obstetrics. But even for our standard “382.01: Acute suppurative otitis media with spontaneous rupture of ear drum” ICD-9 code, we will have to include a side and a timing when converting to “H66.014: Acute suppurative otitis media with spontaneous rupture of eardrum, recurrent, right ear” in ICD-10.
To assist with the conversion, CMS has developed a tool called General Equivalence Mapping, or GEM, which aids in the conversion from a code in ICD-9 to ICD-10, and is available online. This can be a straightforward, one-to-one conversion, or a more complicated one-to-many mapping. GEMs have been created for both a forward mapping ICD-9 to ICD-10 conversion, or a backward mapping ICD-10 to ICD-9 conversion.
What Will This Cost My Practice?
Potential costs of the conversion can vary widely, depending on your IT and administrative support. Providers should plan for an initial decrement in their productivity of five percent to 10 percent during coding functions. If your coding is done for you in your office or the hospital, estimates suggest a decrease in coder efficiency of 20 to 50 percent initially, depending on the site. Most large EMR systems have a robust plan for administrating the ICD-10 conversion, but for providers with practice-specific technology, or worse yet, homegrown systems; a full IT overhaul may be required due to the dependencies with systems that interact with the EMR.
Training for physicians and staff will be costly and time consuming. The Medical Group Management Association (MGMA) estimates it will cost $84,000 for a three-physician practice to transition to ICD-10 and up to $3 million for large practices. There are multiple educational vendors with prepared materials for your office staff, billers, and us as providers, to review the changes that are specific to your area of expertise. Providers should plan on four to six hours of physician education in order to learn the content.
What Steps Should I Be Taking Now?
Providers should communicate with their office manager or financial support personnel to ask for a risk assessment of their practice. This should include questions such as: What will your coding process entail when you are utilizing ICD-10? How much additional documentation will be required, if any, to substantiate the use of the more granular code? Do you have preference lists that can be updated ahead of time to mitigate the disruption to your practice?
We also recommend that practices contact their payers and ask what type of infrastructure they are creating to assist with the conversion and whether there will be billing implications for the use of generic or unsubstantiated codes. Providers should also ask what percentage of their practice these codes and payers represent, and what they can do ahead of time to decrease revenue disruption. Remember, improving documentation accuracy to levels required for ICD-10 can begin now, even if your coding remains in the ICD-9 system. Other implementation and planning strategies could include the creation of a pilot with your office staff of dual coding to test the systems you’ve put into place or asking a payer to partner with you on a dual coding project ahead of the October 1, 2014, deadline in an effort to work out their own transition complications.
Academy Resources for Transition
In an ongoing effort to prepare and educate members regarding the looming transition to the use of ICD-10 diagnostic codes, the Academy has developed a series of educational articles and a dedicated webpage on www.entnet.org as resources for members. In addition, we are working toward an ongoing initiative to develop new resources for members, which will be rolled out during the remainder of 2013 and the first half of 2014. A miniseminar will take place at the 2013 Annual Meeting & OTO EXPOSM in Vancouver, Canada, which will include presentations by ICD-10 experts.
Currently available Academy ICD-10 resources include:
- What’s New: http://www.entnet.org/Practice/International-Classification-of-Diseases-ICD.cfm
- General Information: http://www.entnet.org/Practice/International-Classification-of-Diseases-ICD.cfm
- ICD-9 to ICD-10 Crosswalk for Top 200 ENT Codes: http://www.entnet.org/Practice/loader.cfm?csModule=security/getfile&PageID=156407
- ICD-9 Coding to the highest level of specificity: http://www.entnet.org/practice/resources/upload/Coordinating%20ICD.pdf
Previous Academy Bulletin Articles include:
- Conforming Your Otolaryngology Documentation to ICD-10: http://bulletin.entnet.org/highlight.aspx?id=2904&p=271
- ICD-10: What it Means for Your Practice: http://bulletin.entnet.org/highlight.aspx?id=3516&p=310
- Preparing for ICD-10: http://bulletin.entnet.org/highlight.aspx?id=3925&p=333
Other materials that may be useful to members seeking additional information include:
- CMS PowerPoint on ICD 10 Transition: http://www.cms.gov/Medicare/Coding/ICD10/Downloads/CMSICD-10Overview.pdf
- CMS Implementation Guide: http://www.cms.gov/Medicare/Coding/ICD10/downloads/ICD10SmallandMediumPractices508.pdf
- CMS Proposed Timelines for Small, Medium, and Large Practices: http://www.cms.gov/medicare/coding/ICD10/Downloads
- AMA ICD Transition White Papers: http://www.ama-assn.org/ama/no-index/about-ama/icd10-white-paper-confirmation.page
- AAPC PowerPoint on Transition: http://www.cms.gov/Medicare/Coding/ICD10/Downloads/AAPCICD-10WillChangeEverything.pdf
- AAPC FAQ: http://www.aapc.com/icd-10/faq.aspx#why
- Understanding and Preparing for ICD-10: Making the Conversion from ICD-9 to ICD-10 Manageable: http://www.mgma.com/workarea/downloadasset.aspx?id=1368339