EHR—Meaningful? Useful?
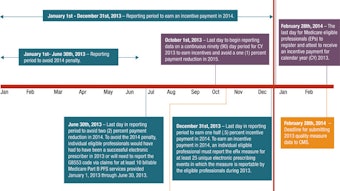
Every president of the United States since George H.W. Bush has touted the electronic health information record (EHR) as the entry point to a new age of healthcare delivery and patient care. The adoption of EHR had been phlegmatic until President Barack Obama initiated and signed into law the American Recovery and Reinvestment Act of 2009. It was this legislation that committed a $20 billion investment in the Health Information Technology for Economic and Clinical Health (HITECH) Act, with the goal of coordinating an informatics infrastructure that would help to eliminate waste and redundancy, enhance quality and safety, allow for improved data collection and analysis, leading to the development of best practices for defined disease entities, i.e., acceptable outcomes for most patients, the most number of times for the least cost. It would therefore result in improved patient care and lower cost, with an anticipated savings of $12 billion over 10 years. In 2010, only 20 percent of physicians and 10 percent of hospitals were using EHR systems.1 The Medicare and Medicaid EHR Incentive Program component of HITECH provided a financial incentive to physicians to buy into the process, with a federally funded “reimbursement” to offset some of the cost of EHR implementation. Of course these funds came with a quid pro quo; physicians had to meet certain criteria in data collection, services and information exchange (Meaningful Use-MU) as a prerequisite for payment. Also, payments to the physicians are staggered over five years, with the criteria for funding not fully developed. Impressively, physicians responded like lemmings jumping off the Norwegian cliffs. The U.S. Department of Health and Human Services boasts that physicians meeting at least five of the core Meaningful Use objectives has increased by at least 66 percent and currently, half of all physicians are meeting nine of the Meaningful Use objectives.2 Two-thirds of physicians have received MU incentives. Now CMS is developing post payment MU audits, using outsourced recovery services, to expose any fraud and abuse. MU will enter Stage 2 in 2014, with a three-month reporting period. The added criteria for Stage 2 were decided upon by identifying the Clinical Quality Measures least reported by current users. The Big Question The biggest frustration of this program is finding the meaning and usefulness of much of the data being collected. Currently, there is no connectivity between practitioners and, other than improved report generation and computer initiated faxing or email, there is no ability to share data. Some federally funded state health information exchange initiatives are being developed, but have been limited to electronic access to laboratory and radiology studies. In the face of this failure to communicate, much of the data collected is moot, with no apparent utility. The next goal of the program is to add PQRS and ICD-10 to our EHR agenda, piling on more administrative strain and another potential roadblock for financial reimbursement from third party payers, including CMS. Where have there been improvements from EHR to date? The ability to send a clinical visit summary to other providers is simplified and expedited. The patients can also be given a written summary of their visit as they exit. Patient healthcare information forms can be developed and personalized, including pre-and post-operative instructions, informed consent, specific disease educational material, and specific therapy material. The added capacity for medication interaction identification and e-prescribing through the Rx component of the EHR enhances patient safety and convenience by eliminating drug interactions and prescribing errors due to handwriting misreads. The next steps should include either a centralization of computer languages or, more likely, super software to allow interconnectivity of all EHR software. Additional services could also be developed. Our Hopes, Our Needs Thomas Goetz, editor of Wired magazine, sponsored and developed an improved clinical laboratory study patient data form, presented on the TEDMED Conference website. He presents a data form that summarizes all normal findings by system, e.g., thyroid, cardiac, and liver all normal. The program then presents abnormal values on a color-coded scale, which explains personal risk to the patient. The program then integrates the lab data with demographics and further develops actions that could be taken for the individual patient. This provides a basis for enhanced patient-doctor interaction, allowing for improved compliance and outcomes. This program costs all of $10,000 for Wired to develop.3 It is time for us, as end-users of EHR, to interact with software companies and the government to put the “meaning” and “useful” into Meaningful Use, put the “quality” into Physician Quality Reporting, and truly improve the quality of patient care. For more information and key dates for CMS Quality Reporting Initiatives, see page 20. Sources Flanders, Adam; “The Real Meaning behind Meaningful Use,” radiographics.rsna.org. US Department of Health and Human Services; “More doctors are adopting EHRs to improve patient care and safety,” HHS.gov/news/press/12/201212b.html. Goetz, Thomas; “It’s time to redesign medical records,” TEDMED, posted 10/11.

The Big Question
The biggest frustration of this program is finding the meaning and usefulness of much of the data being collected. Currently, there is no connectivity between practitioners and, other than improved report generation and computer initiated faxing or email, there is no ability to share data. Some federally funded state health information exchange initiatives are being developed, but have been limited to electronic access to laboratory and radiology studies. In the face of this failure to communicate, much of the data collected is moot, with no apparent utility. The next goal of the program is to add PQRS and ICD-10 to our EHR agenda, piling on more administrative strain and another potential roadblock for financial reimbursement from third party payers, including CMS.
Where have there been improvements from EHR to date? The ability to send a clinical visit summary to other providers is simplified and expedited. The patients can also be given a written summary of their visit as they exit. Patient healthcare information forms can be developed and personalized, including pre-and post-operative instructions, informed consent, specific disease educational material, and specific therapy material. The added capacity for medication interaction identification and e-prescribing through the Rx component of the EHR enhances patient safety and convenience by eliminating drug interactions and prescribing errors due to handwriting misreads. The next steps should include either a centralization of computer languages or, more likely, super software to allow interconnectivity of all EHR software. Additional services could also be developed.
Our Hopes, Our Needs
Thomas Goetz, editor of Wired magazine, sponsored and developed an improved clinical laboratory study patient data form, presented on the TEDMED Conference website. He presents a data form that summarizes all normal findings by system, e.g., thyroid, cardiac, and liver all normal. The program then presents abnormal values on a color-coded scale, which explains personal risk to the patient. The program then integrates the lab data with demographics and further develops actions that could be taken for the individual patient. This provides a basis for enhanced patient-doctor interaction, allowing for improved compliance and outcomes. This program costs all of $10,000 for Wired to develop.3
It is time for us, as end-users of EHR, to interact with software companies and the government to put the “meaning” and “useful” into Meaningful Use, put the “quality” into Physician Quality Reporting, and truly improve the quality of patient care.
For more information and key dates for CMS Quality Reporting Initiatives, see page 20.
Sources
- Flanders, Adam; “The Real Meaning behind Meaningful Use,” radiographics.rsna.org.
- US Department of Health and Human Services; “More doctors are adopting EHRs to improve patient care and safety,” HHS.gov/news/press/12/201212b.html.
- Goetz, Thomas; “It’s time to redesign medical records,” TEDMED, posted 10/11.