Proposed CY 2014 Medicare Physician Fee Schedule (MPFS): What Does It Mean for You?
On July 8, the Centers for Medicare & Medicaid Services (CMS) posted the proposed Medicare physician fee schedule (MPFS) for calendar year (CY) 2014. In addition to payment policy and payment rate updates, the MPFS addresses a number of quality initiatives. The Academy will submit comments to CMS on the proposed rule by the September 6 deadline. The Academy also developed a member summary, which can be accessed here: http://bit.ly/CMSregs. Key provisions Members should be aware of from the proposed rule include: Medicare Sustainable Growth Rate (SGR) Formula The overall estimated impact of the policy changes within the proposed rule for CY 2014 MPFS on otolaryngology is -2 percent. [Note: This amount does not include the possible 24 percent reduction to the conversion factor (CF) that could result if Congress does not take action to prevent the annual cuts from the SGR]. As in years prior, it is expected that Congress will take action to avoid the impending cut before the January 1, 2014 deadline. The Academy continues to campaign for a permanent repeal and replacement of the SGR formula, and has submitted comments on the recent SGR repeal and payment reform legislation. Practice Expense One of the biggest changes in the proposed rule is CMS’ suggestion to change to the methodology for setting practice expense RVUs for services under the PFS. Specifically, they propose that for PFS services provided in the physician offices whose payment rates exceed payment for the same procedure when performed in a facility (hospital outpatient department (HOPD) or Ambulatory Surgical Center (ASC)), CMS would use current year OPPS or ASC rates as a point of comparison in establishing PE RVUs for services in the office under the PFS. For services on the ASC list, they would make the same comparison except they would use the ASC rate as the point of comparison instead of the OPPS rate. In these cases, CMS proposes to limit the office PE RVUs for individual codes so that the total office PFS payment amount would not exceed the total combined amount Medicare pays for the same code in the facility (hospital or ASC) setting. Of note, this policy will severely affect several key Otolaryngology services and the Academy plans to submit comments to CMS on this issue. See the Academy’s summary for a full analysis of impact on ENT service here http://bit.ly/entPEchart. Requirements for Billing “Incident To” Services CMS proposes to revise its regulations to require that individuals performing “incident to” services meet any applicable requirements to provide the services, including licensure imposed by the state in which the services are being furnished. CMS says this will not only provide health and safety benefits to the Medicare patient population, but also assure that federal dollars are not expended for services that do not meet the standards of the states in which they are being furnished. This change will also allow CMS to recover federal government funds paid where services and supplies are not furnished in accordance with state law. This will affect Otolaryngology offices providing incident to services, thus we encourage all practices to ensure their non-physician providers are in compliance with state licensure requirements, to allow for appropriate Medicare reimbursement for the services they provide. Physician Quality Reporting System (PQRS) CMS proposes many overarching changes to the PQRS system, highlights of those affecting otolaryngology are below: As a direct result of Academy advocacy during the past several years, CMS proposes inclusion of four of the Academy Sinusitis Measures for reporting in 2014. CMS proposes eliminating two measures applicable to otolaryngology and eliminating the claims based reporting option for two additional measures applicable to otolaryngology. CMS proposes increasing the number of measures Eligible Professionals (EPs) must report on to qualify for an incentive payment in CY 2014, from three to nine measures. CMS proposes to remove the option of reporting via administrative claims for CY 2014 reporting. CMS proposes to reduce the percentage of patients EPs must report on using a registry from the previous 80 percent down to 50 percent for CY 2014. As indicated below, physicians are eligible to receive a .5 percent incentive payment, or could be subject to a two percent penalty, assessed in 2016, based upon PQRS reporting in 2014. It is important to note these penalties and incentives are separate from other programs such as the EHR Meaningful Use, Electronic Prescribing, and Value Based Payment Modifier programs. Physician Compare Website Recently, CMS released a redesigned Physician Compare website that includes a physician’s address, education and ABMS board certification information, hospital affiliations, and EPs’ language skills. CMS is required to post the names of EPs who satisfactorily report under PQRS and those who are successful e-prescribers under the Medicare eRx Incentive Program. CMS intends to place a check mark moving forward for any individual who has earned a Maintenance of Certification additional Incentives starting with data reported for CY 2013. CMS also plans to post 2014 PQRS GPRO performance data and data from the CG-CAHPS surveys for group practices of 100 or more EPs reporting data under the GPRO in 2013, and for ACOs participating in the MSSP in 2014. For future years CMS proposes to post adding performance rates on measures and patient experience survey measures such as Clinicians and Group Consumer Assessment of Health Providers and Systems (CG-CAHPS) for groups participating in the and Accountable Care Organization (ACO) programs. These proposed changes will likely affect otolaryngology-head and neck surgeons as more information regarding the public’s opinion of the quality of care they received will be posted. The information available on the website is populated automatically from CMS’ PECOS system, so it is critical that members verify their information is accurate. Visit the Physician Compare website at http://www.medicare.gov/physiciancompare. For additional information on what CMS intends to post in future years, access the full Academy summary at http://bit.ly/CMSregs. Electronic Health Record (EHR) Incentive Program CMS proposes that EPs may use the new qualified clinical data registry (QCDR) mechanism to report clinical quality measures that meet both EHR Meaningful Use and PQRS reporting specifications. The measures included in a QCDR are not required to be approved by the National Quality Forum (NQF). Aligning with proposed changes to PQRS reporting, EPs would report nine Clinical Quality Measures (CQMs) included in the Stage 2 final rule covering at least three domains. The Academy is reviewing the requirements to determine if this may be a feasible avenue for otolaryngologists use in the future and will be commenting on the proposal. Value Based Payment Modifier & Physician Feedback Program CMS proposes expanding the Value Based Payment Modifier (VBPM) to groups of 10+ EPs in CY 2014. The VBPM is based on PQRS participation. Groups would report via GPRO-web interface, qualified registries, EHRs, or individually if 70 percent of all EPs in the group report successfully. 2014 reporting will be used to determine whether a payment penalty will apply in CY 2016. CMS plans on expanding the VBPM to all EPs by 2017. An outline of how the program will coincide with PQRS, and how payment adjustments or incentives will be allocated, is below. Members should also know that as of September 16, groups of 25+ will receive physician feedback reports based on their 2012 PQRS performance. For a more detailed explanation, view the Academy’s Value Based Payment Modifier webpage at http://bit.ly/entVBPM. For a more detailed summary on the proposed requirements for the programs highlighted above, visit the Academy’s CMS Regulations page at http://bit.ly/CMSregs or email questions to Academy health policy staff at HealthPolicy@entnet.org.
On July 8, the Centers for Medicare & Medicaid Services (CMS) posted the proposed Medicare physician fee schedule (MPFS) for calendar year (CY) 2014. In addition to payment policy and payment rate updates, the MPFS addresses a number of quality initiatives. The Academy will submit comments to CMS on the proposed rule by the September 6 deadline. The Academy also developed a member summary, which can be accessed here: http://bit.ly/CMSregs. Key provisions Members should be aware of from the proposed rule include:
Medicare Sustainable Growth Rate (SGR) Formula
The overall estimated impact of the policy changes within the proposed rule for CY 2014 MPFS on otolaryngology is -2 percent. [Note: This amount does not include the possible 24 percent reduction to the conversion factor (CF) that could result if Congress does not take action to prevent the annual cuts from the SGR]. As in years prior, it is expected that Congress will take action to avoid the impending cut before the January 1, 2014 deadline. The Academy continues to campaign for a permanent repeal and replacement of the SGR formula, and has submitted comments on the recent SGR repeal and payment reform legislation.
Practice Expense
One of the biggest changes in the proposed rule is CMS’ suggestion to change to the methodology for setting practice expense RVUs for services under the PFS. Specifically, they propose that for PFS services provided in the physician offices whose payment rates exceed payment for the same procedure when performed in a facility (hospital outpatient department (HOPD) or Ambulatory Surgical Center (ASC)), CMS would use current year OPPS or ASC rates as a point of comparison in establishing PE RVUs for services in the office under the PFS. For services on the ASC list, they would make the same comparison except they would use the ASC rate as the point of comparison instead of the OPPS rate. In these cases, CMS proposes to limit the office PE RVUs for individual codes so that the total office PFS payment amount would not exceed the total combined amount Medicare pays for the same code in the facility (hospital or ASC) setting. Of note, this policy will severely affect several key Otolaryngology services and the Academy plans to submit comments to CMS on this issue. See the Academy’s summary for a full analysis of impact on ENT service here http://bit.ly/entPEchart.
Requirements for Billing “Incident To” Services
CMS proposes to revise its regulations to require that individuals performing “incident to” services meet any applicable requirements to provide the services, including licensure imposed by the state in which the services are being furnished. CMS says this will not only provide health and safety benefits to the Medicare patient population, but also assure that federal dollars are not expended for services that do not meet the standards of the states in which they are being furnished. This change will also allow CMS to recover federal government funds paid where services and supplies are not furnished in accordance with state law. This will affect Otolaryngology offices providing incident to services, thus we encourage all practices to ensure their non-physician providers are in compliance with state licensure requirements, to allow for appropriate Medicare reimbursement for the services they provide.
Physician Quality Reporting System (PQRS)
CMS proposes many overarching changes to the PQRS system, highlights of those affecting otolaryngology are below:
- As a direct result of Academy advocacy during the past several years, CMS proposes inclusion of four of the Academy Sinusitis Measures for reporting in 2014.
- CMS proposes eliminating two measures applicable to otolaryngology and eliminating the claims based reporting option for two additional measures applicable to otolaryngology.
- CMS proposes increasing the number of measures Eligible Professionals (EPs) must report on to qualify for an incentive payment in CY 2014, from three to nine measures.
- CMS proposes to remove the option of reporting via administrative claims for CY 2014 reporting.
- CMS proposes to reduce the percentage of patients EPs must report on using a registry from the previous 80 percent down to 50 percent for CY 2014.
As indicated below, physicians are eligible to receive a .5 percent incentive payment, or could be subject to a two percent penalty, assessed in 2016, based upon PQRS reporting in 2014. It is important to note these penalties and incentives are separate from other programs such as the EHR Meaningful Use, Electronic Prescribing, and Value Based Payment Modifier programs.
Physician Compare Website

For future years CMS proposes to post adding performance rates on measures and patient experience survey measures such as Clinicians and Group Consumer Assessment of Health Providers and Systems (CG-CAHPS) for groups participating in the and Accountable Care Organization (ACO) programs. These proposed changes will likely affect otolaryngology-head and neck surgeons as more information regarding the public’s opinion of the quality of care they received will be posted. The information available on the website is populated automatically from CMS’ PECOS system, so it is critical that members verify their information is accurate. Visit the Physician Compare website at http://www.medicare.gov/physiciancompare.
For additional information on what CMS intends to post in future years, access the full Academy summary at http://bit.ly/CMSregs.
Electronic Health Record (EHR) Incentive Program
CMS proposes that EPs may use the new qualified clinical data registry (QCDR) mechanism to report clinical quality measures that meet both EHR Meaningful Use and PQRS reporting specifications. The measures included in a QCDR are not required to be approved by the National Quality Forum (NQF). Aligning with proposed changes to PQRS reporting, EPs would report nine Clinical Quality Measures (CQMs) included in the Stage 2 final rule covering at least three domains. The Academy is reviewing the requirements to determine if this may be a feasible avenue for otolaryngologists use in the future and will be commenting on the proposal.
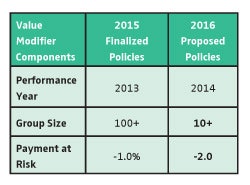
Value Based Payment Modifier & Physician Feedback Program
CMS proposes expanding the Value Based Payment Modifier (VBPM) to groups of 10+ EPs in CY 2014. The VBPM is based on PQRS participation. Groups would report via GPRO-web interface, qualified registries, EHRs, or individually if 70 percent of all EPs in the group report successfully. 2014 reporting will be used to determine whether a payment penalty will apply in CY 2016. CMS plans on expanding the VBPM to all EPs by 2017.
For a more detailed explanation, view the Academy’s Value Based Payment Modifier webpage at http://bit.ly/entVBPM.
For a more detailed summary on the proposed requirements for the programs highlighted above, visit the Academy’s CMS Regulations page at http://bit.ly/CMSregs or email questions to Academy health policy staff at HealthPolicy@entnet.org.