Practice Profile: Working to Improve Healthcare in Our Community
Douglas D. Backous, MD, has a large ear and neurotology practice with Proliance Surgeons at Puget Sound ENT in Edmonds, Washington. He performs inpatient and skull base surgery at the Swedish Neuroscience Institute in Seattle, as well as outpatient otologic surgery in Edmonds and at a satellite facility, Ear Nose and Throat Associates, in Puyallup.
Douglas D. Backous, MD, has a large ear and neurotology practice with Proliance Surgeons at Puget Sound ENT in Edmonds, Washington. He performs inpatient and skull base surgery at the Swedish Neuroscience Institute in Seattle, as well as outpatient otologic surgery in Edmonds and at a satellite facility, Ear Nose and Throat Associates, in Puyallup.
 Douglas D. Backous, MD
Douglas D. Backous, MDHe is the director of the Seattle Advanced Otology Fellowship, which produces one graduate annually. Dr. Backous is Director-at-Large (Private Practice) on the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) Board of Directors and was previously Chair of the AAO–HNS Hearing Committee and Skull Base Surgery Committee.
“I consider my ability to be an otolaryngologist both a privilege and a responsibility,” Dr. Backous explains. “I went to college at Seattle Pacific University to play intercollegiate soccer, having no idea that I would meet professors there who would encourage me to think big and discover a dream to pursue.”
While performing home nursing duties as a work-study student, he met a patient with terminal ALS who motivated him to become a doctor and serve others with respect and dignity. At the University of Washington School of Medicine, Dr. Backous met Charles W. Cummings, MD, who modeled for him how otolaryngology was fun, challenging, and a place to make a difference. During residency at Baylor College of Medicine, he learned the ins and outs of practicing ENT and connected with influential mentors.
“Dr. Herman Jenkins and Dr. Newton Coker opened my eyes to neurotology and guided me to Johns Hopkins University in Baltimore. There, I was reunited with Dr. Cummings to complete my fellowship under Dr. Lloyd Minor and Dr. John Niparko, two mentors who taught me how I could most effectively contribute to our specialty. This incredible opportunity revealed what a responsibility I have, and that we all have, to give back to otolaryngology and work to improve healthcare in our community.”
 Dr. Douglas D. Backous teaching at Miyazaki University, Japan, August 2019
Dr. Douglas D. Backous teaching at Miyazaki University, Japan, August 2019In 1997, Dr. Backous made a difficult decision to leave full-time academic medicine to serve his home community back in the Pacific Northwest. “Most of the referrals I receive come from other otolaryngologists in and around Washington, Alaska, Idaho, and northern Oregon,” he says. “I host regional and online education forums for otolaryngologists, audiologists, and primary care physicians to give back to those who refer to me. My goal in regional education is to make advanced ENT care available closer to patients’ homes by partnering with local physicians. I also co-host the nationally subscribed Seattle Advanced Otology and Rhinology course annually at the Seattle Science Foundation with my practice partner in Puyallup, Dr. Greg Davis.”
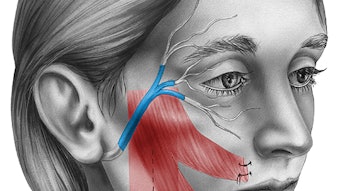
In his practice, Dr. Backous provides leading-edge treatments for pediatric and adult patients with hearing loss, deafness, chronic ear infection, cholesteatoma acoustic neuromas, and facial nerve disorders. His professional passion is ensuring access to care for patients who choose to hear with cochlear implants, brainstem implants, osseointegrated devices, and hearing aids.
Regarding the COVID-19 pandemic, Dr. Backous feels that otolaryngologists need to lead the way for safer in-office and surgical care delivery. “We are uniquely suited, due to our balance of office-based and operating room-based care, to inform industry and develop products that are safer for caregivers and patients,” he says. “We can create clinical pathways for safer care of the upper aerodigestive tract where many viruses and pathogens concentrate.”
In an AAO–HNS COVID-19 podcast on “Reopening Your Practice,” Dr. Backous describes that at least half of his regional neurotology practice patients come from two to three hours away, some by plane. Video conferencing has become an important tool during the pandemic. Under current regulations, similar reimbursement for coding is applied to appropriate clinical evaluations online. “We came up with a physical exam that includes patients taking their own pulse and respiration. It is surprising how many people have their own oxygen saturation monitors and blood pressure cuffs at home.” Practitioners can then bill on key elements or by time spent in medical decision-making and counseling, even justifying level four consults.
 Dr. Douglas D. Backous as a keynote speaker at MedTech Rising in Cork, Ireland, December 2018
Dr. Douglas D. Backous as a keynote speaker at MedTech Rising in Cork, Ireland, December 2018“I recently did consultation leading to eventual emergency surgery on a patient with an acoustic neuroma and brainstem compression. The patient was completely evaluated and consented by me and the neurosurgeon using video conferencing. We met the patient in person the morning of surgery. I see telemedicine as a huge piece to my practice moving forward to help shrink the waiting room while providing essential access to patients at a distance or to those who cannot easily come to the office for care.”
Dr. Backous feels that the Academy’s response during the COVID-19 pandemic is an example of how we as a specialty can mobilize our resources, as well as our resourcefulness, to provide relevant information and care in a timely fashion to support our members and patients in the United States and abroad. “I have always valued the AAO–HNS as an organization that looks out for me and my ability to practice. The educational opportunities, governmental advocacy, and attention to the health and welfare of otolaryngology cannot be overstated.”
Young members who would like to grow into Academy leadership should heed the advice that Dr. Cummings provided Dr. Backous during his fellowship. He suggested volunteering for tasks at the committee level and then delivering on those commitments. Getting involved with the Board of Governors at the state and local levels is a great place to start and is filled with mentoring opportunities as well.
He adds that the Academy can grow by embracing members from different generations and ethnicities to ensure programs exist to provide opportunities for future leaders to learn and be mentored. “The Board and senior leadership team constantly seek ways to hear from members to define the Academy’s direction and purpose.”