Eustachian Tube Dysfunction: Evidence and Controversies
Eustachian tube dysfunction (ETD) is a common diagnosis in general otolaryngology practice. Most patients present with mild symptoms of aural fullness, hearing loss, tinnitus, and otalgia. Despite the prevalence of ETD in children, a standardized approach to diagnosis and management in the adult patient has been lacking.
Edward D. McCoul, MD, MPH
Eustachian tube dysfunction (ETD) is a common diagnosis in general otolaryngology practice. Most patients present with mild symptoms of aural fullness, hearing loss, tinnitus, and otalgia. Despite the prevalence of ETD in children, a standardized approach to diagnosis and management in the adult patient has been lacking. A Clinical Consensus Statement sponsored by the American Academy of Otolaryngology–Head and Neck Surgery Foundation has recently summarized the published evidence for the practicing clinician and forms the basis for the following discussion.
The most common form of ETD is obstructive ETD, defined as the impaired ability to equalize pressure between the middle ear and nasopharynx. The diagnostic approach should focus on ruling out other causes of similar symptoms, including temporomandibular joint disorders, endolymphatic hydrops, and patulous ETD. Chronic otitis media, tympanic membrane perforation, and cholesteatoma are direct sequellae of chronic ETD and may require specialized management.
Key components of the clinical workup include: 1) history, including the ability to perform a modified Valsalva maneuver; 2) pneumatic otoscopy; 3) impedance audiometry; 4) nasal endoscopy; and 5) patient-reported symptom assessment. Although many patients experience persistent symptoms, some individuals are symptomatic only during periods of barochallenge such as diving or air travel. Otoscopy may show reduced tympanic membrane mobility, middle ear effusion, or chronic changes to the tympanic membrane. Impedance audiometry (or tympanometry) provides a quantitative measure of middle ear ventilation, which indirectly reflects Eustachian tube function. A significant limitation is that tympanometry may be falsely negative if the patient is asymptomatic at the time of the test.
Nasal endoscopy should not be overlooked as it allows the identification of extrinsic causes of ETD, such as adenoid hypertrophy or a nasopharyngeal mass. Endoscopy also can identify inflammation at the Eustachian tube nasopharyngeal orifice, which may indicate the presence of allergic rhinitis, chronic rhinosinusitis, or extra-esophageal reflux. In these cases, medical management of the comorbid inflammatory disease is warranted before considering additional intervention aimed at the Eustachian tube.
Patient-reported outcome measures are useful for summarizing symptom burden and providing a benchmark for tracking a patient’s course of symptoms over time. The 7-item Eustachian Tube Dysfunction Questionnaire (ETDQ-7) is a validated instrument that has been used in clinical studies and can be readily incorporated into clinical practice.
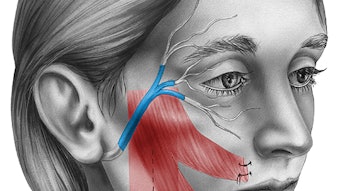
While the history of Eustachian tube surgery dates back nearly 200 years, the past 20 years have seen a resurgence of interest in treatments aimed at modifying the structure and function of that organ. Treatments including laser ablation, mucosal tissue removal, and cartilaginous reshaping have been suggested. More recently, balloon dilation of the Eustachian tube (BDET) has emerged as a treatment option. In BDET, a catheter with a balloon is temporarily inserted and inflated within the cartilaginous portion of the Eustachian tube. Multiple devices are now available with FDA labeling for the treatment of obstructive ETD.
The need for radiologic imaging prior to BDET has been debated. While the proximity of the carotid canal to the bony Eustachian tube has been noted, the current generation of FDA-approved devices includes design elements that prevent advancement of the instrument beyond the cartilaginous portion of the lumen. A dehiscent carotid artery identified on imaging is a contraindication to use of a device without a depth marker.
Controversy exists regarding the full range of indications for BDET. At a minimum, current evidence suggests that BDET may be offered to patients with chronic symptoms (three months or greater) with elevated symptom scores (i.e., ETDQ-7), persistent middle ear effusion or non-adherent atelectasis, abnormal tympanometry, and inflammation at the Eustachian tube orifice. Patients with a strong history of intermittent symptoms on barochallenge and signs of Eustachian tube inflammation may also be good candidates for BDET. It is unclear whether symptomatic patients without objective abnormalities may benefit from BDET, as several studies have shown mixed results.
Randomized controlled trials have demonstrated subjective and objective improvements in 55% to 70% of patients undergoing BDET with topical nasal steroid compared to those receiving topical nasal steroid alone. These results seem to be durable up to 12 months following the procedure. Technical aspects related to the duration of dilation and the ideal setting for this procedure remain to be determined. Success with BDET is likely to be predicated upon conscientious patient selection and a focus on patient-reported symptoms.
Myringotomy with tympanostomy has been the mainstay for surgical management of obstructive ETD for decades. Although tympanostomy tubes do not directly remedy the dysfunction at the Eustachian tube, they provide reliable symptom relief and should be offered along with BDET as alternative therapies. However, myringotomy with or without tympanostomy tube placement is not a mandatory prerequisite to offering BDET. In cases where a functioning tympanostomy tube fails to relieve symptoms of ETD, an alternative diagnosis should be sought.
Adjunctive procedures may have a role in treating obstructive ETD. Adenoidectomy may be useful to eliminate extrinsic compression from a large central adenoid pad. The presence of adenoid tissue arising from the mucosa of the torus tubarius may lend itself to endoscopic ablation, though evidence for this and other adjunctive procedures is lacking. Select patients with chronic ear pathology may be candidates for BDET at the time of middle ear surgery.
Amid growing interest in ETD as a clinical entity, further investigation should expand the evidence base and guide the clinician in the diagnosis and management of this common condition. The coming years are likely to witness a deepening appreciation of the pathophysiology of obstructive ETD and lead to new avenues for medical and surgical treatment.
Presented at the AAO-HNSF 2019 Annual Meeting & OTO Experience in New Orleans, LA
References:
- Tucci DL, McCoul ED, Rosenfeld RM, et al. Clinical consensus statement: Balloon dilation of the Eustachian tube. Otolaryngol Head Neck Surg. 2019;161(1):6-17.
- McCoul ED, Anand VK, Christos PA. Validating the clinical assessment of Eustachian tube dysfunction: The Eustachian Tube Dysfunction Questionnaire (ETDQ-7). Laryngoscope 2012;122(5):1137-41.
- Poe D, Anand V, Dean M, et al. Balloon dilation of the eustachian tube for dilatory dysfunction: A randomized controlled trial. Laryngoscope. 2018;128(5):1200-1206.
- Anand V, Poe D, Dean M, et al. Balloon dilation of the Eustachian tube: 12-month follow-up of the randomized controlled trial treatment group. Otolaryngol Head Neck Surg. 2019;160:687-94.
- Cutler JL, Meyer TA, Nguyen SA, O’Malley EM, Thackeray L, Slater PW. Long-term outcomes of balloon dilation for persistent Eustachian tube dysfunction. Otol Neurotol. 2019;40:1322-25.