Bridging the gap
On April 27, 2016, the Centers for Medicare & Medicaid Services (CMS) released the proposal for the long-awaited replacement for the Sustainable Growth Rate (SGR) as the payment system for physicians participating in Medicare: the Merit-based Incentive Payment System (MIPS) and Alternative Payment Model (APM) programs.
New CMS payment system provides two paths for quality reporting: the Merit-based Incentive Payment System (MIPS) and Alternative Payment Model (APM)

Under the MIPS, starting January 1, 2017, physicians will report on four categories that add up to a composite score that CMS will use to determine whether or not Eligible Clinicians (ECs), including most otolaryngologist-head and neck surgeons, receive a bonus payment or are subject to a payment reduction in 2019 and beyond. According to the Brookings Institution: “Under the new MIPS program, physicians report to the government payer directly (CMS) and receive a bonus or penalty based on performance on measures of quality, resource use, meaningful use of electronic health records [now known as Advancing Care Information (ACI)], and Clinical Practice Improvement Activities (CPIA). The bonus or payment reduction physicians may see starts at 4 percent of the fee schedule in 2019 (based on their performance two years prior—in this case 2017) and increases successively to 5 percent in 2020, 7 percent in 2021, and 9 percent from 2022 forward. From 2026 onward, MIPS providers would receive an annual increase of 0.25 percent on their base fee schedules rates.”
MIPS

Resource Use: 10 percent of composite score
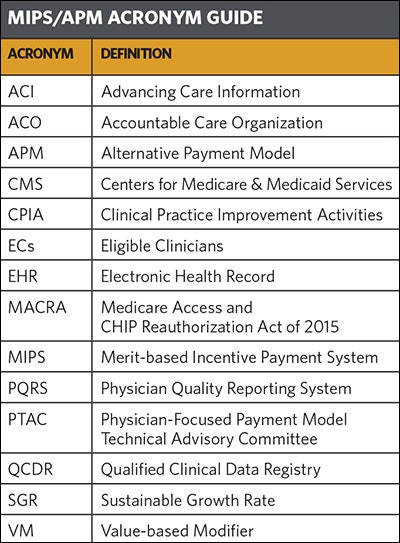
Quality: 50 percent of composite score
The quality category will replace the PQRS program and account for 50 percent of an EC’s composite score for the first year. ECs will report a minimum of six measures with at least one cross-cutting measure and one outcome measure, if available. If an outcome measure is not available, ECs can report one other high priority measure. MIPS ECs will be able to use a qualified registry, a qualified clinical data registry (QCDR) such as RegentSM, or an electronic health record (EHR) to report quality measures.
CPIA: 15 percent of composite score
CPIA (Clinical Practice Improvement Activities) is a new category under MIPS and accounts for 15 percent of an EC’s composite score for the first year. CPIA allows physicians to select from a list of more than 90 activities to receive credit for this category. ECs can report CPIA through a qualified registry, an EHR system, a QCDR such as RegentSM, the CMS web interface, and attestation data submission.
ACI: 25 percent of composite score
The Advancing Care Information component will replace the EHR Meaningful Use program and account for 25 percent of an EC’s composite score for the first year. MIPS ECs will report measures to form a base score and performance score. Unlike the all-or-nothing scoring in the Meaningful Use program, ECs can receive partial credit for the ACI portion of the MIPS composite score. ECs can use a qualified registry, EHR system, QCDR such as RegentSM, attestation, and CMS web interface submission methods to report ACI measures.
APMs
A small number of physicians are exempted from the MIPS by participating in an Advanced APM. Advanced APMs defined as those that meet criteria for linking payments to quality measures, using EHRs, and bear more than a nominal financial risk. Participants who meet the strict Advanced APM criteria would be eligible for a 5 percent bonus payment from CMS on top of any incentives built into the Advanced APM model. Current APMs that meet Advanced APM criteria are Track 2 & 3 Accountable Care Organizations (ACOs), Next Generation ACOs, Comprehensive Primary Care Plus, and some Comprehensive End State Renal Disease Care Organizations.
In addition to Advanced APMs, there are several other APMs available to ECs including MIPS APMs, which provide more favorable MIPS composite scoring, and Physician-Focused Payment Models, which are submitted to the Physician-Focused Payment Models Technical Advisory Committee (PTAC). Due to the restrictive Advanced APM definition, the Academy does not expect that many otolaryngologist-head and neck surgeons will be able to participate in the Advanced APM program for the first few years. However, the Academy is working with the American College of Surgeons in addition to other stakeholders to evaluate and hopefully develop APMs that will help otolaryngologist-head and neck surgeons participate in Physician-Focused Payment Models, MIPS APMs, and hopefully Advanced APMs in the future. Members can access more information on APMs and the Academy’s efforts by accessing www.entnet.org/content/alternative-payment-models.
Academy staff and physician leaders are currently reviewing the extensive proposal and will advocate for continued progress toward a less burdensome reporting system that truly incorporates quality of care for patients into payment while still allowing for necessary reporting flexibility. Although the Academy believes the MIPS and APM programs are a start in the right direction, CMS can continue to work with otolaryngologist-head and neck surgeons to allow for the widest range of innovative ideas to ensure the greatest numbers of physicians are able to not only participate, but succeed in these future payment models. The Academy met with CMS in May and plans on submitting comments. Once submitted, the Academy will make these comments available to all Members. Members should look out for the comment letter in the News, HP Update, and on the Academy’s website at www.entnet.org/content/physician-payment-reform.