Global Surgical Outreach for Cleft and Craniofacial Conditions
A recent survey maps the current landscape of humanitarian work addressing cleft and craniofacial conditions in low- and middle-income countries worldwide.
Ryan H. Belcher, MD, MPH, Steven Goudy, MD, MBA, and Travis T. Tollefson MD, MPH, on behalf of the Cleft and Craniofacial Committee
Otolaryngologists and Global Surgical Care

Recently our group—comprising members of the AAO-HNS Cleft and Craniofacial and Humanitarian Efforts committees together with the American Academy of Facial Plastic and Reconstructive Surgery (AAFPRS)—have endeavored to establish a "hub" of information on otolaryngology teams' efforts across the globe. Our aim is to enable each volunteer organization to efficiently and accurately identify other teams that are aligned in their goals, their collaborations, and their region of interest.
Challenges in Cleft Care Access
Patients affected by cleft lip and cleft palate in LMICs often lack access to specialized surgical care owing to lack of awareness, financial burdens that prevent families from seeking care, and inadequate numbers of trained surgeons in their region. A recent survey of the otolaryngology-head and neck surgery global workforce showed that the otolaryngology-head and neck surgery workforce in LMICs is less than one surgeon per 100,000 population, compared to over five surgeons per 100,000 in high-income countries.¹ Otolaryngology-head and neck surgery specialists were reported to perform 20% of the cleft lip and palate surgical care in the LMICs that were surveyed, indicating the significant global impact of otolaryngology-head and neck surgery in cleft care.¹
Models of Care Delivery
There is no one-size-fits-all model for global surgical humanitarian work, and approaches are often shaped by long-standing personal relationships combined with the dynamics and needs of each country. There are certainly instances where a humanitarian surgical endeavor is unidirectional, in which patients receive surgical care from a volunteer team that has traveled to deliver the care with limited local interactions. This unidirectional or vertical model of care delivery has been de-emphasized over the last two decades in favor of a bidirectional model. The bidirectional model involves collaboration with local medical personnel with the aim to educate, empower, and equip to fill the necessary local voids. Partnerships between high-income countries and LMICs should be designed to be sustainable with capacity building for the local healthcare delivery systems.
Work by Otolaryngology-Head and Neck Surgeons
Recently, the AAO-HNS Cleft and Craniofacial Committee developed a survey to gather data on outreach efforts in the cleft and craniofacial space. As an initial assessment, 37 respondents from 30 US-based institutions were recruited from the members of the AAO-HNS and the AAFPRS. These respondents performed surgical outreach efforts in 19 countries across Africa, Europe, the Caribbean, Asia, and Central and South America. Most of the outreach efforts were sponsored by nonprofit organizations.
Many of these efforts can be found on the AAO-HNS Humanitarian Efforts interactive map.
We ask that you submit information about your global surgical efforts and organization at this website if it is not already listed.
Survey Results and Findings
Diving further into the data from the survey showed the duration of each global surgery outreach had a median of seven days (range 5–14 days). The exception was a surgeon who is working to build capacity in a hospital in East Africa, where 210 patients underwent surgery over 162 days. Table 1 shows the organizations involved with each humanitarian trip and the surgical concentrations for the trip.
Table 1. Procedures and Interventions treated by different organizations.
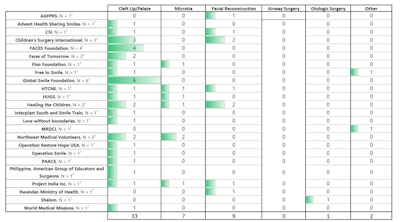
Most of the respondents (n = 33/37; 78%) concentrated on cleft lip and palate surgery. Facial reconstruction was the primary objective in ten (32%) out of the 37 initiatives, while, more specifically, microtia care was involved in seven (19%) of the 37. Several teams included microvascular reconstruction and otology care. As far as priorities, training of local surgeons was prioritized in the majority (n = 26/37; 70%) of the outreach initiatives, and US-based residents and fellows participated in more than half (n = 24/37; 65%) of the initiatives. Figure 1 shows a map of the world with the countries represented by the trips taken and number of patients surgically treated.
 Figure 1. Number of patients treated across the world.
Figure 1. Number of patients treated across the world.
Future Directions
The aim of this survey was to examine the current state of otolaryngology-head and neck surgery international cleft and craniofacial outreach initiatives as a collaboration between the AAFPRS and the AAO-HNS's Humanitarian Efforts and Otolaryngology Cleft and Craniofacial committees. Despite the success of the global surgery outreach efforts in expanding access to otolaryngology-head and neck surgery care, the unmet burden of surgical disease requires a creative reshaping of the "medical mission" models into more diagonal and/or bidirectional models of care delivery and collaborations.¹'² The data collected can act as a starting point to help coordinate future efforts in supporting host country surgeons and surgical systems seeking to improve otolaryngology-head and neck surgery care in LMICs.³ The otolaryngology-head and neck surgery community contributes significantly to global cleft and craniofacial care, and our committee will establish a website for all surgical teams to register and seek domestic and international partnerships to address our shared goals.
References
- Petrucci B, Okerosi S, Patterson RH, Hobday, Salano V, Waterworth CJ, Brody RM, Sprow H, Alkire BC, Fagan JJ, et al. "The Global Otolaryngology-Head and Neck Surgery Workforce." JAMA Otolaryngology–Head and Neck Surgery 149, no. 10 (2023): 904-911.
- Belcher R, Patel K, Clark J, Horne S. "Addressing Cleft Care in Low- and Middle-Income Countries Beyond Cleft Lip and Palate with Improvement of Otolaryngology, Audiology, and Speech Services." Cleft Palate-Craniofacial Journal (2025). Online ahead of print. https://doi.org/10.1177/10556656251319649.
- Magro I, Sharma R, Goudy S, Tollefson TT, Belcher R. "The State of Otolaryngology-Head and Neck Surgery Efforts in Global Surgery Outreach: Initiatives to Address Cleft Lip-Palate and Craniofacial Care." Facial Plastic Surgery & Aesthetic Medicine (2025).


















