Reg-ent Registry Insights: Chronic Rhinosinusitis
Reg-ent registry analysis examines trends in the prevalence of CRS and its treatment patterns.
Vikas Mehta, MD, MPH, Coordinator for Research and Quality, Kristine Schulz, DrPH, MPH, AAO-HNSF Senior Director for Research and Quality, Soniya Phatak, MPH, Senior Manager, Reg-ent Registry, Samuel Kim, BS, AAO-HNSF Data Analyst, Reg-ent Registry, Jocelyn Meyer, MPH, AAO-HSNF Reg-ent Registry Director, Jenel Lansang, MSN, RN, AAO-HNSF Reg-ent Registry Senior Manager
If you’re attending the AAO-HNSF 2025 Annual Meeting & OTO EXPOSM, be sure to visit the Research and Quality booth to interact with the chronic rhinosinusitis dashboard, compare results to balloon sinuplasty, and explore other intriguing analyses!

The American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO-HNSF) developed a comprehensive clinical practice guideline focused on the surgical management of adult CRS with the goal to identify opportunities for quality improvement and to provide clinicians with trustworthy, evidence-based recommendations to enhance patient outcomes, reduce practice variation, and ensure safe, effective care.
Based on the key action statements recommended in the guideline to assess the patient and the case for antibacterial therapy and candidacy for surgery, the Reg-ent team conducted a deeper analysis of registry data to examine trends in the prevalence of CRS and its treatment patterns, specifically focusing on the use of ESS and antimicrobial therapy.
Materials and Methods
The initial patient population for this study was derived from the Reg-ent database and included patients aged 18 years and older diagnosed with CRS. The total study population included 531,109 patients with a CRS diagnosis. To define CRS, we used a comprehensive set of 36 diagnostic codes including both ICD-9 and 10, which encompasses both acute and chronic forms of sinusitis, including site-specific classifications such as maxillary, frontal, ethmoidal, sphenoidal, and pansinusitis. The study period for CRS diagnoses spanned from 2019 to 2023.
From the CRS population, we identified a subset of patients who subsequently underwent ESS. ESS procedures were identified using a range of CPT codes that captured various surgical nasal and sinus endoscopies, including partial and total ethmoidectomies (with or without frontal sinus exploration or sphenoidotomy), maxillary antrostomies (with or without tissue removal), frontal sinus explorations, and sphenoidotomies (with or without tissue removal). To ensure adequate follow-up, ESS procedures were included through the end of 2024 to allow for one calendar year of observation following CRS diagnoses made in 2023.
Lastly, from the ESS cohort, we then identified a final cohort of patients who received an antimicrobial order associated with their ESS procedure. Antimicrobial receipt was determined based on orders placed in any perioperative timeframe—including preoperative, intraoperative, or postoperative periods—surrounding the ESS procedure episode. The observation window for antimicrobial prescriptions was defined as up to 13 weeks to encompass the preoperative, intraoperative, and postoperative prescriptions.
Results
From the initial CRS population, we stratified patients based on treatment pathways and identified 32,720 (8.8%) patients who underwent ESS. Within the ESS cohort, 60.3% (19,724) of patients were prescribed antimicrobial therapy as part of the perioperative regimen.
To better understand diagnostic patterns for the CRS population, we analyzed the most frequently used ICD-9 and ICD-10 codes from 2019 to 2023. Within this timespan, we observed an overall increase in the number of CRS patients captured in the dataset—from 112,370 patients in 2019 to 218,402 patients in 2023. From the Reg-ent database, we identified 36 diagnosis codes applicable to CRS, with J32.0 (chronic maxillary sinusitis) emerging as the most widely charted code, accounting for 26.2% of all CRS diagnoses. Other commonly charted diagnosis codes included both ICD-9 and ICD-10 classifications for acute and chronic sinusitis, as well as recurrent sinusitis, and site-specific conditions such as sphenoid and maxillary sinusitis. Additionally, the ICD-10 code J32.9, representing unspecified chronic sinusitis, accounted for 21% of all CRS diagnoses.
From the CRS population, we conducted a descriptive analysis of patient demographics. Our preliminary analysis of CRS trends revealed that individuals aged 60–69 years had the highest rate of diagnosis within the Reg-ent dataset, accounting for 21.5% of the total patient population. This was followed by the 50–59-year age group at 18.8%. In terms of gender distribution, most patients diagnosed with CRS were female (59.7%), compared to male (40.3%).
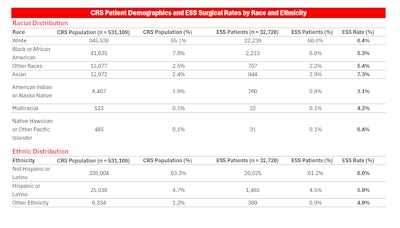
Table. CRS Patient Demographics and ESS Surgical Rates by Race and Ethnicity summarizes the racial and ethnic distribution of the CRS population alongside those who underwent ESS.
Regionally, the distribution of CRS population was as follows: Mid-Atlantic (32.4%), South Atlantic (28.7%), South Central (18.4%), Midwest (8.1%), Pacific (5.5%), New England (3.6%), and Mountain (2.7%). A notably high concentration of CRS diagnoses was observed in Mid-Atlantic states such as New York (20.6%) and New Jersey (9.0%), as well as in South Central and South Atlantic states including Texas (8.8%), South Carolina (7.0%), Florida (6.8%), and North Carolina (5.7%).
In terms of the ESS cohort, geographic distribution revealed that the South Atlantic region had the highest prevalence of ESS at 29.7%, followed by the Mid-Atlantic region (24.4%) and the South Central region (21.0%). The Pacific (8.6%), Mountain (4.1%), and New England (3.4%) regions had the lowest ESS prevalence rates.
The Reg-ent registry receives data from participating EHR systems with patient demographic information occasionally incomplete or unavailable, which may result in demographic percentages not adding to 100%.
As per the clinical practice guidelines, ESS has been commonly used to treat CRS. Our analyses were designed to address the research needs identified in the CPG to enhance knowledge of the CRS disease profile, as well as explore patterns of antimicrobial use during CRS treatment.
Temporal trends from 2019 to 2024 showed ESS rates rising from 7.7% in 2019 to a peak of 9.9% in 2021, before declining to 7.2% by 2023. During this same period, the number of patients diagnosed with CRS increased significantly—from 112,370 in 2019 to 218,402 in 2023—indicating that the decline in ESS rates occurred despite a growing CRS patient population.
We conducted a focused analysis of ESS cohort from 2019 to 2024 to examine the distinct combinations of sinus cavities treated across all ESS procedures. This patient-level analysis evaluated all procedure episodes per individual, identified every unique nasal cavity that was operated on, and grouped patients based on the full set of sinus cavities treated throughout their surgical history. Across all sinus cavity combinations, we identified 15 unique sinus cavity groupings, with the most frequent being all four sinuses (31%), followed by ethmoid and maxillary (25.3%), maxillary only (13.6%), and ethmoid, frontal, and maxillary (13.2%). In contrast, the frontal and sphenoid sinuses represented the least common combination occurring in just 0.2% of cases.
We further analyzed the ESS cohort at the patient-level to determine the maximum number of sinus cavities treated during any single procedure episode for each individual patient. Among all patients, the most frequent maximum involved all four sinus cavities, observed in 30.8% of cases, followed by two cavities (29.7%), three cavities (21.6%), and one cavity (17.9%).
Detailed analysis revealed a positive correlation between the number of sinus cavities treated and the rate of antimicrobial use. Procedures involving a single sinus cavity like maxillary, ethmoid, sphenoid, or frontal were associated with an average antimicrobial prescription rate of 54.5%. Antimicrobial prescription rates were elevated in multi-cavity procedures with an average documented antimicrobial prescription rate of 61.5%. The highest antimicrobial prescription rate, 65%, was observed in cases involving all four sinus cavities: ethmoid, frontal, maxillary, and sphenoid.
 Figure. ESS & Antibiotic Patient Counts with Antibiotic Order Rate.
Figure. ESS & Antibiotic Patient Counts with Antibiotic Order Rate.
Preoperatively, amoxicillin was the most prescribed antimicrobial, followed by doxycycline and sulfamethoxazole/trimethoprim. Ciprofloxacin had the lowest preoperative prescription rate. Significantly, preoperative antimicrobial use was higher than intraoperative and postoperative use across both single and multi-cavity procedures. Amoxicillin was also the most frequently prescribed antimicrobial in the intraoperative setting, followed by cefazolin and doxycycline. In the postoperative period, doxycycline was the most prescribed antimicrobial. Across all timepoints, we identified the 10 most typically prescribed antimicrobials from our dataset, with amoxicillin ranking first, followed by doxycycline and sulfamethoxazole/trimethoprim. Zithromax had the lowest prescription rate over the entire study period.
To assess whether antimicrobial receipt was associated with reoperation, we first examined procedure episodes across the entire cohort. At the patient level, we identified the total number of procedure episodes per individual, which ranged from one to four. Within the ESS cohort (n = 32,270), the majority of patients (95%, or 31,183) had only one procedure episode. Among these patients, the perioperative documented antimicrobial prescription rate was 59.7%. As the number of procedure episodes increased, we observed a positive relationship between procedure frequency and antimicrobial use: patients with two procedure episodes had a documented antimicrobial prescription rate of 71.4%, those with three procedures had a rate of 75.2%, and those with four procedures had a rate of 96%.
We then analyzed the remaining 1,537 patients (4.7%) who underwent two or more ESS procedure episodes during the study period. For this group, we examined documented antimicrobial prescription patterns across multiple procedure episodes, with a specific focus on whether antimicrobials were prescribed in the perioperative period of any procedure prior to the patient's last ESS episode. For example, in patients with two procedure episodes, we assessed whether an antimicrobial was prescribed around their first procedure episode; for patients with three or four procedure episodes, we evaluated whether antimicrobials were prescribed around any of their previous procedures (i.e., the first and/or second dates, depending on total number of procedure episodes).
 Figure. ESS Cohort: Antibiotics Ordered Prior to Latest ESS.
Figure. ESS Cohort: Antibiotics Ordered Prior to Latest ESS.
These results may reflect differing clinical practices or case complexity in patients who undergo multiple ESS procedures. Antimicrobial receipt was coded as a binary indicator: a patient was classified as “antimicrobial ordered” if they had at least one antimicrobial order at any previous ESS procedure dates in that window, even if subsequent dates lacked orders.
Discussion
CRS is an increasingly significant health concern both in the United States and globally. In the U.S., approximately 11.5% of adults report symptoms consistent with CRS.4,5 Beyond its high prevalence, CRS has a significant impact on quality of life, equally burdensome to other chronic conditions. It is also associated with increased healthcare costs and reduced overall productivity.1
In response to these challenges, the Reg-ent team conducted an in-depth analysis to explore trends in CRS prevalence and treatment patterns and evaluate research gaps identified in the recently published CPG guideline using data collected from the Reg-ent registry database. The CPG specifically highlighted critical areas where further research is needed, particularly in relation to patient demographic characteristics, treatment outcomes, and the comparative effectiveness of different surgical and medical treatment options over time.
As indicated in the results section, our analysis revealed that ESS was considered the most widely accepted and used treatment for CRS, along with medical therapy. While it has been established as an important step in managing CRS, the overall trend in surgeries performed over time shows a decline post- pandemic. Several factors may explain this decline. During the post pandemic in the clinical setting, several physicians saw a significant reduction in ESS procedures. In a survey of rhinologists,7 60% of respondents (n= 277) indicated they had performed no endoscopies during the initial phases of the pandemic. The authors also noted less than 20% of the number of pre-pandemic nasal endoscopies performed in the post-pandemic period.6
The heterogeneity of CRS with multiple phenotypes and endotypes, such as milder or non-polypoid CRS, may be effectively managed with non-surgical options such as topical saline irrigations, intranasal corticosteroids, and other medical therapies. Biological therapies have demonstrated increased efficacy in reducing polyp burden, improving symptoms, and reducing the need for revision surgery. It is also important to note that the study cohort was limited to outpatient data, which may have contributed to the observed reduction in procedural volumes and prescriptions.
A parallel decline in antimicrobial prescriptions was also observed during this period. Regarding antimicrobial utilization, amoxicillin was the most frequently prescribed agent, which aligns with its favorable pharmacologic profile, broad-spectrum coverage, and established efficacy in CRS management. However, our analysis also revealed a notable level of doxycycline use in postoperative settings. Although not considered a first-line agent for all CRS cases, doxycycline offers a clinically valuable alternative to macrolides, particularly in patients with macrolide intolerance, resistance, or in scenarios where its anti-inflammatory properties may benefit postoperative recovery. Based on the data, it is evident that antimicrobial stewardship in CRS perioperative care is vital to balance the risks and benefits of antimicrobial use.
Conclusions
As chronic rhinosinusitis (CRS) continues to represent a significant and growing public health concern, understanding how the treatment patterns correlate with patient outcomes is critical to ensuring that treatment strategies should continue to be effective and efficient. Evaluation of the long-term effectiveness of surgical interventions, the appropriateness and impact of various antimicrobial regimens is critical. Extensive, longer prospective studies are required to analyze and identify gaps in CRS care and treatment. With antimicrobials use, due to the variability in practice, further rigorous research is needed to clarify the use of antimicrobials, to optimize patient outcomes and combat antimicrobial resistance.
While this study primarily analyzed observed data trends, our team’s future work will focus on a detailed evaluation of the cohort to address questions outlined in the Clinical Practice Guideline. Specifically, we aim to assess the efficacy of targeted antimicrobials, the impact of biologic therapies, and the role of imaging findings in influencing surgical outcomes. The goal of our team is to work with our practices and providers to integrate these insights into an evidence-based framework to promote more personalized and value-driven care for our patients, while supporting broader public health goals and refining the power of our specialty.
Note: The data presented in this study are derived from the Reg-ent clinical data registry, which collects clinical information from participating in private practices and academic medical centers. As such, the dataset may not reflect a comprehensive or nationally representative sample. Patient demographics and counts may be disproportionately influenced by the geographic distribution and characteristics of participating sites. Therefore, the findings should be interpreted as trends observed within the Reg-ent dataset and not as indicative of broader, nationwide patterns.
References
- Surgical Management of Chronic Rhinosinusitis. Otolaryngol Head Neck Surg. 2025;00(00):1–47. doi:10.1002/ohn.1287. Available at: http://otojournal.org
- Centers for Disease Control and Prevention. Sinus infection (sinusitis). U.S. Department of Health & Human Services. Published 2020. Accessed April 19, 2024. https://www.cdc.gov/nchs/fastats/sinuses.htm
- Denneny JC III, Cyr DD, Witsell DL, Brereton J, Schulz KA. A pathway to value‐based care of chronic rhinosinusitis using a claims database. Laryngoscope Investig Otolaryngol. 2019;4(1):193‐206. doi:10.1002/lio2.232
- Centers for Disease Control and Prevention. FastStats—sinus conditions. Published January 27, 2022. Accessed April 19, 2024. https://www.cdc.gov/nchs/fastats/sinuses.htm#print
- National Center for Health Statistics. Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2012. Published 2014.
- Patel R, Huang A, Lin A, et al. COVID-19 and rhinological surgery. Oper Tech Otolaryngol Head Neck Surg. 2022;33(2):103-111.
- Papagiannopoulos P, Ganti A, Kim YJ, et al. Impact of COVID-19 pandemic on ambulatory and operating room rhinology practice in the US. American Journal of Rhinology & Allergy. 2021; 35:441–448. doi: 10.1177/1945892420961962.