A Better Night’s Sleep: Advances in Therapy for Sleep Apnea
Well-established therapies continue to provide relief for many patients with obstructive sleep apnea.
Reena Dhanda Patil, MD, on behalf of the General Otolaryngology and Sleep Medicine Education Committee

Fortunately, certain well-established therapies continue to provide relief for many patients with OSA. For example, treatment of nasal obstruction is recognized to be critical in preventing downstream collapse of the pharyngeal airway and may even decrease snoring and mildly improve OSA. Expansion of the nasal valve utilizing radiofrequency ablation or a lateral nasal wall implant such as Latera® (Stryker) are more recent techniques to improve the nasal airway.2 Positional therapy also remains a mainstay, although efforts to encourage non-supine sleep (e.g., the “tennis ball technique”) can be plagued by low compliance. However, new vibrotactile wearable devices may be used to comfortably avoid supine sleep without arousing patients unnecessarily.
Interestingly, a recent trend shows movement back toward pharyngoplasty techniques popularized by Ted Fujita in the 1980s.3 However, a more advanced understanding of anatomic collapse in OSA has resulted in a shift from resective surgeries, such as Fujita’s classic uvulopalatopharyngoplasty (UPPP), to more reconstructive procedures, such as expansion sphincter pharyngoplasty (ESP) and barbed reposition pharyngoplasty (BRP). In particular, the BRP uses barbed suture placed along various points of the lateral pharyngeal wall to create tension and widen the airway dimensions, especially the retropalatal airway.4 Another area of the oropharynx that can be addressed is the base of tongue, especially when obstructive lingual tonsillar hypertrophy is present. This area is notoriously difficult to access, and innovative surgical approaches have been developed to improve its exposure, such as transoral robotic surgery. See photos of the barbed reposition pharyngoplasty technique in Iannella et al. 2022.4
Skeletal surgery also benefits from newer approaches to time-honored techniques; for example, Airlift® (Siesta Medical) for hyoid suspension allows for predictable advancement of the hyoid anteriorly and superiorly to expand the hypopharyngeal airway.5 For more invasive skeletal surgery, maxillomandibular advancement remains a highly efficacious OSA treatment. However, more minimal approaches to maxillary or mandibular deficiency, such as palatal expansion, can be pursued non-invasively via our orthodontic colleagues for patients unwilling to undergo more extensive surgery.
Hypoglossal nerve stimulation (HGNS) continues to rise globally. The Inspire® (Inspire Medical) device, which remains the only U.S. Food and Drug Administration (FDA)-approved device at time of publication, has been performed over 100,000 times globally and is now an established treatment in terms of efficacy and patient acceptance. Recent expansion of FDA guidelines and a more streamlined surgical approach with Inspire V will likely fuel continued interest from patients seeking HGNS.6 Current research in this field increasingly focuses on “soft criteria” for implantation, recognizing that device effectiveness relies on adequate patient usage which can be affected by myriad comorbid sleep and psychiatric disorders.
Despite these available effective therapies, demand for more innovation within the landscape of OSA treatment continues to rise. Additional options that may define the future of OSA treatment include:
Weight loss drugs (GLP-1 agonists) are a tremendously popular way to shed pounds and improve OSA. Although bariatric surgery remains a mainstay of weight management, many are turning to pharmacotherapy as a more expeditious and less invasive weight management strategy. We see this especially with the recent FDA approval of tirzepatide (Zepbound®) for OSA; currently it is best understood that its mechanism of OSA improvement is primarily driven by weight loss, although there may be other effects that are not yet elucidated.7
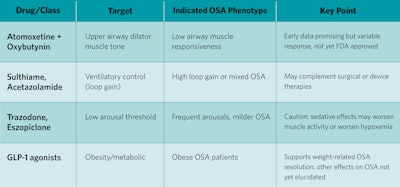
Other pharmacotherapy agents aim to address specific nonanatomic OSA endotypes, such as high loop-gain, inadequate upper airway dilator muscle function, and low arousal threshold (Table 1). Carbonic anhydrase inhibitors, such as acetazolamide, can be used for high loop-gain to improve the body’s ventilatory response to changes in blood levels of carbon dioxide. Another drug in trials is AD109, a combination of atomoxetine (a norepinephrine reuptake inhibitor) and oxybutynin (an anticholinergic), which has shown promise in promoting upper airway dilator muscle tone during sleep. Finally, attention is being paid to hypnotic medications, such as eszoplicone or trazodone, which may elevate the arousal threshold, especially in patients for whom “light sleep” contributes to cortical arousals and central sleep apnea.8 See Table 1 below.
Table 1. Pharmacotherapy for OSA.
Myofunctional therapy (MT) is recognized as a promising treatment for patients who do not wish to pursue traditional therapies for OSA. This therapy, typically administered by speech pathologists or dentists, promotes exercises targeting the tongue, soft palate, and pharyngeal muscles to strengthen the upper airway muscles and reduce collapsibility.9 Although not a primary treatment for severe OSA, MT may benefit those with mild disease or serve as an adjunct to other therapies.
Advances in neurostimulation continue to be pursued by investigators and manufacturers in the U.S. and internationally. HNGS devices already available in Europe are currently awaiting FDA approval, including Genio® (Nyxoah) and aura6000 (LivaNova).10-11 In addition, others are trialing ansa cervicalis stimulation to promote downward tension on the thyroid cartilage and prevent collapsibility of the pharyngeal airway.12 This area of sleep surgery is quite popular, and start-up companies are looking at neurostimulation delivery options from every angle.
Management of OSA has evolved dramatically beyond CPAP and UPPP. We now have an expanding toolbox of surgical, device-based, and pharmacologic interventions to offer patients when they are referred for CPAP intolerance. Notably, patients may benefit from a combination of treatments to suit their individual OSA phenotype. With enhanced knowledge of our patients’ anatomic collapse patterns and physiologic endotypes, we can use cutting-edge therapies in a personalized fashion to help our patients sleep better.
References
- Surani S, Taweesedt P. Obstructive Sleep Apnea: New Perspective. Medicina (Kaunas). 2022 Dec 29;59(1):75. doi: 10.3390/medicina59010075. PMID: 36676699; PMCID: PMC9862185.
- Kim DH, Lee HH, Kim SH, Hwang SH. Effectiveness of using a bioabsorbable implant (Latera) to treat nasal valve collapse in patients with nasal obstruction: systemic review and meta-analysis. Int Forum Allergy Rhinol. 2020 Jun;10(6):719-725. doi: 10.1002/alr.22543. Epub 2020 Apr 13. PMID: 32282129.
- Fujita S, Conway W, Zorick F, Roth T: Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 1981;89:923-934.
- Iannella G, Lechien JR, Perrone T, Meccariello G, Cammaroto G, Cannavicci A, Burgio L, Maniaci A, Cocuzza S, Di Luca M, Stilo G, De Vito A, Magliulo G, Greco A, de Vincentiis M, Ralli M, Pelucchi S, Ciorba A, Vicini C. Barbed reposition pharyngoplasty (BRP) in obstructive sleep apnea treatment: State of the art. Am J Otolaryngol. 2022 Jan-Feb;43(1):103197. doi: 10.1016/j.amjoto.2021.103197. Epub 2021 Sep 1. PMID: 34492427.
- Van Tassel J, Chio E, Silverman D, Nord RS, Platter D, Abidin MR. Hyoid Suspension With UPPP for the Treatment of Obstructive Sleep Apnea. Ear Nose Throat J. 2023 May;102(5):NP212-NP219. doi: 10.1177/01455613211001132. Epub 2021 Mar 18. PMID: 33734881.
- https://www.inspiresleep.com/en-us/how-inspire-therapy-works/
- Malhotra A, Grunstein RR, Fietze I, Weaver TE, Redline S, Azarbarzin A, Sands SA, Schwab RJ, Dunn JP, Chakladar S, Bunck MC, Bednarik J; SURMOUNT-OSA Investigators. Tirzepatide for the Treatment of Obstructive Sleep Apnea and Obesity. N Engl J Med. 2024 Oct 3;391(13):1193-1205. doi: 10.1056/NEJMoa2404881. Epub 2024 Jun 21. Erratum in: N Engl J Med. 2024 Oct 17;391(15):1464. doi: 10.1056/NEJMx240005. PMID: 38912654; PMCID: PMC11598664.
- Lee YC, Lu CT, Chuang LP, Lee LA, Fang TJ, Cheng WN, Li HY. Pharmacotherapy for obstructive sleep apnea - A systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2023 Aug;70:101809. doi: 10.1016/j.smrv.2023.101809. Epub 2023 Jun 17. PMID: 37423095.
- Saba ES, Kim H, Huynh P, Jiang N. Orofacial Myofunctional Therapy for Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. Laryngoscope. 2024 Jan;134(1):480-495. doi: 10.1002/lary.30974. Epub 2023 Aug 22. PMID: 37606313.
- Woodson BT, Suurna MV, Gillespie MB, Huntley TC, Hancock M, Santos A, Subbaroyan J, Makori F, Fesneau G, Heiser C, Kent DT. Multicentre study conducted across centres in the USA, Europe and Australia to assess the safety and effectiveness of a bilateral hypoglossal nerve stimulation system for the treatment of obstructive sleep apnoea in adults: a protocol for a pivotal, multicenter, open-label, single-arm study. BMJ Open. 2024 Dec 20;14(12):e085218. doi: 10.1136/bmjopen-2024-085218. PMID: 39806685; PMCID: PMC11667466.
- Schwartz AR, Jacobowitz O, Eisele DW, Mickelson SA, Miller MB, Oliven A, Certal V, Hopp ML, Winslow DH, Huntley TC, Nachlas NE, Pham LV, Gillespie MB, Weeks BH, Lovett EG, Shen J, Malhotra A, Maurer JT. Targeted Hypoglossal Nerve Stimulation for Patients With Obstructive Sleep Apnea: A Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg. 2023 Jun 1;149(6):512-520. doi: 10.1001/jamaoto.2023.0161. Erratum in: JAMA Otolaryngol Head Neck Surg. 2024 Jun 1;150(6):530. doi: 10.1001/jamaoto.2024.0412. PMID: 37022679; PMCID: PMC10080405.
- Kent DT, Zealear D, Schwartz AR. Ansa Cervicalis Stimulation: A New Direction in Neurostimulation for OSA. Chest. 2021 Mar;159(3):1212-1221. doi: 10.1016/j.chest.2020.10.010. Epub 2020 Oct 14. PMID: 33065104; PMCID: PMC8097630.