Kids ENT Health Month: Awareness of the dangers of button battery ingestion in children
Over the last few decades, there has been a notable increase in electronics, toys, watches, greeting cards, and other devices powered by button batteries. These seemingly innocuous objects can be found in nearly all households. During the same time period, there has been a dramatic rise in the prevalence of button battery injuries, the overwhelming majority occurring in children.
Ryan H. Belcher, MD; C. Anthony Hughes, MD, MBA, MPH; Rose J. Eapen, MD; Robert H. Chun, MD; Craig S. Derkay, MD

Over the last few decades, there has been a notable increase in electronics, toys, watches, greeting cards, and other devices powered by button batteries. These seemingly innocuous objects can be found in nearly all households. During the same time period, there has been a dramatic rise in the prevalence of button battery injuries, the overwhelming majority occurring in children.
Prior to 1983, there were only six reported cases of button battery ingestion in the scientific literature.1,2 Now in the United States, a child may present to the emergency department for a battery-related complaint as often as every three hours.3
In 2010, the National Capital Poison Center published a seven-fold increased risk of major effect on the morbidity and mortality in button battery ingestions in children compared to previous reported literature.
How does battery ingestion cause complications?
Swallowing a battery or applying a battery to a moist surface (e.g., the ear canal, throat, or the nose) can result in injury because the moisture in these areas can result in leaching of hydroxide from the battery’s negative pole. This will damage and liquefy the lining of the esophagus, nose, or ear drum, resulting in a severe burn or perforation.
If the diagnosis is confirmed with x-ray imaging and/or there is a strong clinical suspicion, emergency removal of the battery is the next step. This is typically managed in the operating room by an otolaryngologist, particularly if the button battery is lodged in the esophagus or airway. The esophagus is the site of the most severe complications because of the moist environment, close proximity of tissues, and slow movement.
Once the battery is removed endoscopically, the physician is encouraged to report the case to the National Battery Ingestion Hotline with the size/type of battery, source of battery, and any available clinical data.5
In delayed button battery removal or significant esophageal injury, an esophagram may be performed before advancing diet, and a “second look” endoscopy two to four days post-removal can be useful in reassessing injury. Children may require careful monitoring to ensure no further injury occurs even after the battery is removed. Vascular injuries have been described, and an MRI of the chest to determine proximity of injury to the aorta or CT angiography to exclude aortic injury may be considered.

What to do if a child ingests a button battery or if there is suspicion of an event
If a caretaker does not witness the ingestion event, it can be hard to diagnose this problem, as the symptoms (e.g., drooling, vomiting, fever, decreased oral intake, difficulty swallowing, cough) may mimic other common disease processes in children, such as viral illnesses. Should there be any suspicion of a button battery ingestion, even if the event is not witnessed, the parent or caretaker should seek immediate medical help in the emergency room setting. If there is a witnessed ingestion, the poison control website (poison.org) has a list of steps to take.
If anyone ingests a battery, this is what you should do:
- Immediately call the 24-hour National Battery Ingestion Hotline at 800-498-8666 (or 202-625-3333).
- If readily available, provide the battery identification number, found on the package or from a matching battery.
- In most cases, an x-ray must be obtained right away to be sure that the battery has gone through the esophagus into the stomach. (If the battery remains in the esophagus, it must be removed immediately. Most batteries move on to the stomach and can be allowed to pass by themselves.) Based on the age of the patient and size of the battery, the National Battery Ingestion Hotline specialists can help you determine if an immediate x-ray is required.
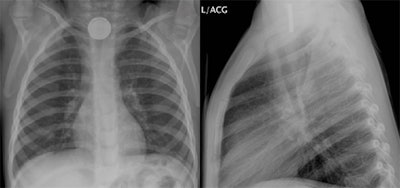
In any cases of clinical suspicion, a simple two-view chest/neck x-ray should be obtained to diagnose and distinguish a button battery with the “double ring” sign from the ingestion of a simple coin. (See Figure 1.)
What are some preventive strategies?
Given the severe complications that ingested button batteries can cause within a short timeframe (two hours), preventive strategies cannot be stressed enough. While the distribution of information and increased awareness of the dangers of button batteries to caregivers, parents, and medical professionals is helpful, these are not sufficient by themselves to prevent injuries. It is believed that securing the battery compartment of the product is the single most important intervention required to prevent battery ingestion injuries.5 Other strategies include avoiding loose or accessible button batteries and redesigning battery packages with child-resistant packaging.5
It is important that parents and caregivers are knowledgeable about which devices and toys require button batteries. Hearing aid batteries are the most frequently reported source of ingested batteries out of all devices. Lithium batteries have become increasingly popular as a result of longer shelf life and increased stability. However, these larger 20mm batteries have an increased voltage (3V) and increased risk of impaction and have also contributed to 94 percent of known battery fatalities.5 Most often these 20mm batteries are used for games and toys, watches and stopwatches, flameless candles, bathroom and kitchen scales, and key fobs.5
What are other areas of concern in the head and neck?
All caretakers and parents should also be aware that children can often place the batteries in the ear or get them lodged in the nose. The corrosive nature of the batteries can destroy the surrounding tissues in these areas and create multiple complications including conductive hearing loss, ear canal stenosis, septal perforation, nasal obstruction, or scar bands. As in the esophagus with ingestions, there is a narrow time window in which the button battery needs to be removed from the ear or nose to avoid catastrophic tissue damage.
For more information on Kids ENT Health Month visit http://www.entnet.org/KidsENT

Bibliography
- Buttazzoni E, Gregori D, Paoli B, et al. Symptoms associated with button batteries injuries in children: an epidemiological review. International journal of pediatric otorhinolaryngology. 2015; 79:2200-2207.
- Reilly D. Mercury battery ingestion. BMJ. 1979; 1:859.
- Sharpe SJ, Rochette LM, Smith GA. Pediatric battery-related emergency department visits in the United States. Pediatrics. 2012; 129(6):1111-1117.
- Poison Control. Swallowed a button battery? Battery in the nose or ear? www.poison.org/battery. Accessed 11/29/17, 2017.
- Jatana KR, Litovitz T, Reilly JS, Koltai PJ, Rider G, Jacobs IN. Pediatric button battery injuries: 2013 task force update. International journal of pediatric otorhinolaryngology. 2013; 77:1392-1399.