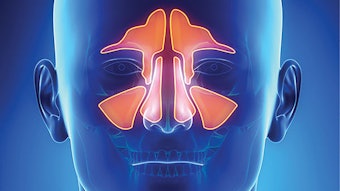
New Clinical Consensus Statement on Balloon Dilation of the Sinuses
The AAO-HNSF’s Otolaryngology–Head and Neck Surgery journal recently published the Clinical Consensus Statement (CCS) on Balloon Dilation of the Sinuses (BDS) that was previewed at our Annual Meeting in Chicago last year.
The AAO-HNSF’s Otolaryngology–Head and Neck Surgery journal recently published the Clinical Consensus Statement (CCS) on Balloon Dilation of the Sinuses (BDS) that was previewed at our Annual Meeting in Chicago last year. I would like to thank and congratulate the participants on the panel that produced the statements of agreement related to this evolving tool for treating disorders of the sinonasal tract.

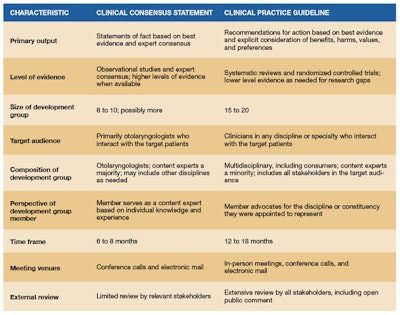
The use of this technology as it continues to evolve has proven to be a valuable addition to the armamentarium of the otolaryngologist treating sinus-related diseases. The Academy felt that it would be beneficial to produce a CCS that describes best practices and current management paradigms based on existing scientific literature and a panel of experts in the field of rhinology. This document would provide guidance to practitioners treating sinus-related disease, patients affected by these diseases, and the payers covering these treatments.
I feel this CCS accomplishes that goal, based on our current knowledge. As the field progresses and further advancements are made, evidence may accumulate that warrants future updates to all or part of this document. As is the case with all our CCS and CPG products, the CCS on BSD will be reviewed on a regular basis and updated based on the most current literature and experience.
The following organizations have endorsed the CCS: American Academy of Allergy, Asthma & Immunology; American Academy of Otolaryngic Allergy; American Rhinologic Society; and the Triological Society.
— James C. Denneny III, MD
Patient criteria
- Balloon dilation is not appropriate for patients who are without both sinonasal symptoms and positive findings on CT.
- Balloon dilation is not appropriate for the management of headache in patients who do not otherwise meet the criteria for chronic sinusitis or recurrent acute sinusitis.
- Balloon dilation is not appropriate for the management of sleep apnea in patients who do not otherwise meet the criteria for chronic sinusitis or recurrent acute sinusitis.
- CT scanning of the sinuses is a requirement before balloon dilation can be performed.
- Balloon dilation is not appropriate for patients with sinonasal symptoms and a CT that does not show evidence of sinonasal disease.
- Balloon dilation can be appropriate as an adjunct procedure to FESS in patients with chronic sinusitis without nasal polyps.
- There can be a role for balloon dilation in patients with persistent sinus disease who have had previous sinus surgery.
- There is a role for balloon sinus dilation in managing patients with recurrent acute sinusitis as defined in the AAO-HNSF guideline based on symptoms and the CT evidence of ostial occlusion and mucosal thickening.
- Surgeons who consider reusing devices intended for dilation of the sinuses should understand the regulations set forth by the FDA for reprocessing such devices and ensure that they are followed.
- Balloon dilation can be performed under any setting as long as proper precautions are taken and appropriate monitoring is performed.
- Balloon dilation can be performed under local anesthesia with or without sedation.
- Balloon dilation can improve short-term quality-of-life outcomes in patients with limited CRS without polyposis.
- Balloon dilation can be effective in frontal sinusitis.
Perioperative considerations
Outcomes