AAO-HNSF CLINICAL CONSENSUS STATEMENTSeptoplasty with or without inferior turbinate reduction
Nasal obstruction is a highly prevalent problem in the United States that can negatively impact quality of life. One of the common causes of nasal obstruction is a deviated septum, with or without hypertrophic inferior turbinates. In the presence of such nasal obstruction, nasal septoplasty and inferior turbinate reduction procedures can improve the nasal airway.
By Joseph K. Han, MD, Scott P. Stringer, MD, Richard M. Rosenfeld, MD, MPH, Timothy S. Lian, MD
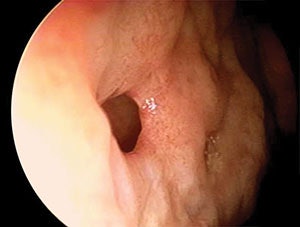 Yanigisawa Image Library: Telescopic view (4mm, 0˚) shows a perforation of the nasal septum in its anterior inferior portion.
Yanigisawa Image Library: Telescopic view (4mm, 0˚) shows a perforation of the nasal septum in its anterior inferior portion.Nasal obstruction is a highly prevalent problem in the United States that can negatively impact quality of life. One of the common causes of nasal obstruction is a deviated septum, with or without hypertrophic inferior turbinates. In the presence of such nasal obstruction, nasal septoplasty and inferior turbinate reduction procedures can improve the nasal airway. Septoplasty can also be used as an adjunctive procedure to improve access to, and the function of, the paranasal sinuses.
Despite a long history of septoplasty as a procedure, there are significant differences of opinion regarding the appropriate methods for diagnosis and treatment of nasal obstruction secondary to septal deviation and turbinate hypertrophy. The roles of nasal endoscopy, imaging, photodocumentation, and tests such as acoustic rhinometry/rhinomanometry in the diagnosis of nasal obstruction are unclear. Payers have imposed requirements for using some of these methodologies prior to approving payment for septal surgery in the absence of appropriate evidence-based literature to support the requirements. Similarly, requirements for extended medical therapy prior to authorization for septoplasty and/or inferior turbinate reduction surgery have been imposed by a number of payers without clear evidence of benefit.
During the development stage of the clinical consensus statement, a complete definition of septoplasty with or without inferior turbinate reduction was established. Additional statements addressing the diagnosis, medical management prior to septoplasty, and surgical considerations, as well as the appropriate role of perioperative, postoperative, and adjuvant procedures, in addition to outcomes, were subsequently produced and evaluated. The end result produced a series of clinical statements, developed by an expert panel, such as CT scan may not accurately demonstrate the degree of septal deviation; septoplasty can assist delivery of intranasal medications to the nasal cavity; endoscope can be used to improve visualization of posterior based septal deviation during septoplasty; and quilting sutures can obviate the need for nasal packing after septoplasty.
The desire to improve quality of care, promote appropriate care, decrease variations in the care of septoplasty patients, and educate clinicians, led the Rhinology and Paranasal Sinus Committee of the American Academy of Otolaryngology-Head and Neck Surgery Foundation (AAO-HNSF) to submit the topic of septoplasty to the AAO-HNSF Guidelines Task Force. Due to the limited evidence to support a guideline in this regard, the topic of septoplasty was selected for clinical consensus statement (CCS) development. The objectives are to promote appropriate care, reduce inappropriate variations in care, and educate clinicians regarding multiple aspects of the medical and surgical management of nasal obstruction employing septoplasty with or without inferior turbinate reduction. A Miniseminar during the AAO-HNSF 2015 Annual Meeting & OTO EXPOSM presented the result of this process, and focuses on diagnosis, medical therapy, and surgical interventions.







