Academics vs. Private Practice: Who’s Suffering Most?
When I finished my fellowship and joined academics more than a decade ago, I was thrilled with the opportunity to teach residents, investigate research ideas, and have job security. The challenges of our changing reimbursement system—new quality measurements, RVU-based incentives, diagnostic codes (ICD-10 & ICD-11), and facility fees for my patients—are affecting my hospital-based practice and generating frustration with my choice of academia. Could it be easier in private practice? Six months ago, while exchanging practice pearls with friends at our state otolaryngology society conference, I heard how private practice is in distress, with the introduction of insurance exchange, increased overhead, EMR expenses, and competition with hospital-based employed otolaryngologists. During this energetic conversation, there was a moment where I felt there may be a growing divide among otolaryngologists where each user of a certain practice model looks at others as “the lucky ones.” Having attended the AAO-HNSF and ACS meetings during the last year, I see high frustration among surgeons. The confusion of a novel healthcare system has left many surgeons feeling excluded from decision-making, knee-deep in bureaucracy, and on their way to an early retirement. I sense a growing rift between private practice surgeons and those who are hospital-based. The issue is plain: How can a private practice survive as hospital systems buy out local otolaryngologists to secure their network and patient stream? Can a private practice endure without ancillary diagnostic and OR revenue that a hospital system already generates? While these questions are provocative, I’m not sure they address the bigger question: Can our American healthcare system survive without any change? The American healthcare system, as complex as it is, still yields the greatest surgical innovations and the largest volume of clinical research in the world. Our otolaryngology residency training system is internationally revered as foremost for efficiently and cost effectively covering the entire spectrum of otolaryngology-head and neck disorders. As you already know, the cost of our system per capita is enormous and growing. Unfortunately, surgeons are a targeted group for expense cutting through pending revaluation of CPT codes and quality-based payment restructuring. Fortunately, I am a member of the AAO-HNS, the only group battling at congressional levels for my vocation. So, as I reflect on my dialogues with colleagues about the frustration of practice, I’m not sure that either private practice or academic surgeons are suffering from a greater disadvantage. We are all faced with mutual adversity and the complexity of a generational movement in our healthcare system. As I look to the future, I will not view my colleagues as a source of frustration, but as my friends to lean on, as we brace together for a rocky road ahead. *Stay alert and connect: bog@entnet.org
 Sanjay R. Parikh, MD
Sanjay R. Parikh, MDBOG Secretary
When I finished my fellowship and joined academics more than a decade ago, I was thrilled with the opportunity to teach residents, investigate research ideas, and have job security. The challenges of our changing reimbursement system—new quality measurements, RVU-based incentives, diagnostic codes (ICD-10 & ICD-11), and facility fees for my patients—are affecting my hospital-based practice and generating frustration with my choice of academia. Could it be easier in private practice?
Six months ago, while exchanging practice pearls with friends at our state otolaryngology society conference, I heard how private practice is in distress, with the introduction of insurance exchange, increased overhead, EMR expenses, and competition with hospital-based employed otolaryngologists. During this energetic conversation, there was a moment where I felt there may be a growing divide among otolaryngologists where each user of a certain practice model looks at others as “the lucky ones.”
Having attended the AAO-HNSF and ACS meetings during the last year, I see high frustration among surgeons. The confusion of a novel healthcare system has left many surgeons feeling excluded from decision-making, knee-deep in bureaucracy, and on their way to an early retirement. I sense a growing rift between private practice surgeons and those who are hospital-based. The issue is plain: How can a private practice survive as hospital systems buy out local otolaryngologists to secure their network and patient stream? Can a private practice endure without ancillary diagnostic and OR revenue that a hospital system already generates? While these questions are provocative, I’m not sure they address the bigger question: Can our American healthcare system survive without any change?
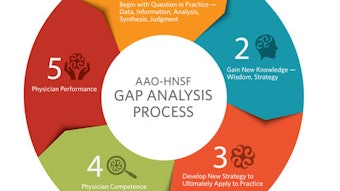
The American healthcare system, as complex as it is, still yields the greatest surgical innovations and the largest volume of clinical research in the world. Our otolaryngology residency training system is internationally revered as foremost for efficiently and cost effectively covering the entire spectrum of otolaryngology-head and neck disorders. As you already know, the cost of our system per capita is enormous and growing. Unfortunately, surgeons are a targeted group for expense cutting through pending revaluation of CPT codes and quality-based payment restructuring. Fortunately, I am a member of the AAO-HNS, the only group battling at congressional levels for my vocation.
So, as I reflect on my dialogues with colleagues about the frustration of practice, I’m not sure that either private practice or academic surgeons are suffering from a greater disadvantage. We are all faced with mutual adversity and the complexity of a generational movement in our healthcare system. As I look to the future, I will not view my colleagues as a source of frustration, but as my friends to lean on, as we brace together for a rocky road ahead.
*Stay alert and connect: bog@entnet.org