William Harry Barnes: Pioneer for the Specialty
Duane J. Taylor, MD Chair, Diversity Committee My deep and committed involvement in the Academy for the past 20+ years has been due in large part to my initial and long-standing involvement as a member of the Board of Governors representing the W. Harry Barnes Society and Otolaryngology Section of the National Medical Association (NMA). The NMA represents the organization of African-American physicians in our specialty. The name William Harry Barnes has most recently been linked with an Academy-sponsored Endowed Leadership Grant to honor his legacy. However, I am sure the majority of our Academy members may ask, “Who was Dr. William Harry Barnes?” Dr. Barnes became the first African-American to be certified by an American specialty board in 1927. That was the year he became a diplomate of the American Board of Otolaryngology. Dr. Barnes was born to a life of humble beginnings in Philadephia in 1887. His desire to become a doctor started at a very young age. In 1908, he graduated from Central High School of Philadelphia with a bachelor of arts degree. After taking a competitive entry exam, he received a four-year scholarship to the University of Pennsylvania Medical School, becoming the first African-American to be awarded this scholarship. In 1912, he received his MD degree and then completed his internship at Douglass and Mercy Hospitals in Philadelphia. He respected the value of hard work and believed education to be an ongoing process. These tenets were a consistent source of his drive and determination for his many accomplishments during his relatively short life. Dr. Barnes had his first appointment as an assistant otolaryngologist at Frederick Douglass Hospital in 1913 in Philadelphia. In 1918, he served as an acting assistant surgeon in the U.S. Public Health Service. Three years later, he took further postgraduate studies in otolaryngology and head and neck surgery at the University of Pennsylvania. He subsequently was appointed chief otolaryngologist of Frederick Douglass Hospital and clinical assistant otolaryngologist at Jefferson Medical School, in Philadelphia in 1916. In 1922, Dr. Barnes announced he would devote his practice exclusively to ear, nose, and throat disorders. Two years later, he was appointed consultant otolaryngologist at Mercy Hospital and desired further training in otolaryngology. Unable to receive this training in the United States, he went to the University of Paris and the University of Bordeaux to undertake more advanced studies during 1924. He found himself studying under Dr. Pierre Sebileau, professeur de la Faculté de médecine de Paris; L. Baldenweck, MD, in Paris; and Dr. Emil-Jean Moure, professor of otology, University of Bourdeaux. After his return to the United States, he took more courses with Dr. Unger in 1926. Dr. Barnes was drawn to the work that Dr. Chevalier Jackson was doing in Philadelphia with bronchoesophagology and studied under him to master this technique. In the early 1930s, he organized and headed the department of bronchoscopy at Mercy Hospital and received an appointment as a lecturer and consultant at Howard University Medical School in Washington, DC, in bronchoscopy. He taught many physicians his techniques and published numerous papers on a variety of topics in the specialty. Dr. Barnes served as the 37th president of the NMA in 1936, the largest organization of African-American physicians in the world. He was the founder of the Society for the Promotion of Negro Specialists in Medicine and served as President of the Philadelphia Academy of Medicine and Allied Sciences. He was a member of the Philadelphia County Medical Society, the Pennsylvania State Medical Society, American Laryngological Association, and the AMA. He also was known as an inventor and innovator. He invented the hypophyscope for visualizing the pituitary through a transeptal approach. He developed an early medical record system and devised instruments for removal of lingual tonsils. He also developed an operative technique for drainage of peritonsillar abscesses and myringotomy. Dr. Barnes was a humanitarian and donated much of his time and talent to those who could not afford care. He was active in his church, serving as the president of the board of trustees of Zoar Methodist Church, and was appointed as one of the original members of the Philadelphia Housing Authority, which he served on until his death. He was married to Mattie Thomas and had five sons, two of whom were physicians. He died January 15,1945, of pneumonia. He was 58. References 1. Cobb, M. Medical History. Journal of the National Medical Association (JNMA).1955 Jan: 64-66. 2. Smith Jr., A.P. The Society for the Promotion of Negro Specialists in Medicine. JNMA. 1954 Jul.
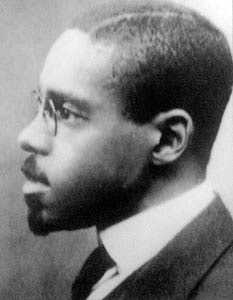 William Harry Barnes, MD, was the first African-American to be certified by an American specialty board when he became a diplomate of the American Board of Otolaryngology in 1927.
William Harry Barnes, MD, was the first African-American to be certified by an American specialty board when he became a diplomate of the American Board of Otolaryngology in 1927.Duane J. Taylor, MD
Chair, Diversity Committee
My deep and committed involvement in the Academy for the past 20+ years has been due in large part to my initial and long-standing involvement as a member of the Board of Governors representing the W. Harry Barnes Society and Otolaryngology Section of the National Medical Association (NMA). The NMA represents the organization of African-American physicians in our specialty. The name William Harry Barnes has most recently been linked with an Academy-sponsored Endowed Leadership Grant to honor his legacy. However, I am sure the majority of our Academy members may ask, “Who was Dr. William Harry Barnes?”
Dr. Barnes became the first African-American to be certified by an American specialty board in 1927. That was the year he became a diplomate of the American Board of Otolaryngology.
Dr. Barnes was born to a life of humble beginnings in Philadephia in 1887. His desire to become a doctor started at a very young age. In 1908, he graduated from Central High School of Philadelphia with a bachelor of arts degree. After taking a competitive entry exam, he received a four-year scholarship to the University of Pennsylvania Medical School, becoming the first African-American to be awarded this scholarship. In 1912, he received his MD degree and then completed his internship at Douglass and Mercy Hospitals in Philadelphia. He respected the value of hard work and believed education to be an ongoing process. These tenets were a consistent source of his drive and determination for his many accomplishments during his relatively short life.
Dr. Barnes had his first appointment as an assistant otolaryngologist at Frederick Douglass Hospital in 1913 in Philadelphia. In 1918, he served as an acting assistant surgeon in the U.S. Public Health Service. Three years later, he took further postgraduate studies in otolaryngology and head and neck surgery at the University of Pennsylvania. He subsequently was appointed chief otolaryngologist of Frederick Douglass Hospital and clinical assistant otolaryngologist at Jefferson Medical School, in Philadelphia in 1916.
In 1922, Dr. Barnes announced he would devote his practice exclusively to ear, nose, and throat disorders. Two years later, he was appointed consultant otolaryngologist at Mercy Hospital and desired further training in otolaryngology. Unable to receive this training in the United States, he went to the University of Paris and the University of Bordeaux to undertake more advanced studies during 1924. He found himself studying under Dr. Pierre Sebileau, professeur de la Faculté de médecine de Paris; L. Baldenweck, MD, in Paris; and Dr. Emil-Jean Moure, professor of otology, University of Bourdeaux. After his return to the United States, he took more courses with Dr. Unger in 1926. Dr. Barnes was drawn to the work that Dr. Chevalier Jackson was doing in Philadelphia with bronchoesophagology and studied under him to master this technique.
In the early 1930s, he organized and headed the department of bronchoscopy at Mercy Hospital and received an appointment as a lecturer and consultant at Howard University Medical School in Washington, DC, in bronchoscopy. He taught many physicians his techniques and published numerous papers on a variety of topics in the specialty.
Dr. Barnes served as the 37th president of the NMA in 1936, the largest organization of African-American physicians in the world. He was the founder of the Society for the Promotion of Negro Specialists in Medicine and served as President of the Philadelphia Academy of Medicine and Allied Sciences. He was a member of the Philadelphia County Medical Society, the Pennsylvania State Medical Society, American Laryngological Association, and the AMA.
He also was known as an inventor and innovator. He invented the hypophyscope for visualizing the pituitary through a transeptal approach. He developed an early medical record system and devised instruments for removal of lingual tonsils. He also developed an operative technique for drainage of peritonsillar abscesses and myringotomy.
Dr. Barnes was a humanitarian and donated much of his time and talent to those who could not afford care. He was active in his church, serving as the president of the board of trustees of Zoar Methodist Church, and was appointed as one of the original members of the Philadelphia Housing Authority, which he served on until his death. He was married to Mattie Thomas and had five sons, two of whom were physicians. He died January 15,1945, of pneumonia. He was 58.
References
| 1. | Cobb, M. Medical History. Journal of the National Medical Association (JNMA).1955 Jan: 64-66. |
| 2. | Smith Jr., A.P. The Society for the Promotion of Negro Specialists in Medicine. JNMA. 1954 Jul. |









