Physician Payment Policy (3P) Workgroup Update: Current Technological Incentive Programs and Upcoming Penalties
Richard W. Waguespack, MD, coordinator for Socioeconomic Affairs and Michael Setzen, MD, coordinator for Practice Affairs, Co-chairs of 3P Health Policy staff: Jean Brereton, senior director, Research, Quality, and Health Policy; Jenna Kappel, director, Health Policy; Jenna Minton, senior manager, Health Policy; Joe Cody, Health Policy analyst; Harrison Peery, Health Policy analyst The Physician Payment Policy Workgroup (3P), co-chaired by Richard W. Waguespack, MD, and Michael Setzen, MD, is the senior advisory body to Academy leadership and staff on issues related to socioeconomic advocacy, regulatory activity, coding or reimbursement, and practice services or management. 3P and the Health Policy staff have been busy in 2012 with a continued high level of activity, constant emails, and monthly calls, working diligently and tirelessly on behalf of all members. Below, we want to draw your attention to the fact that, in the next few years, there will be numerous opportunities through incentives and potential minefields by way of penalties that will affect your practice as technological advances change the way we practice medicine (see Table 1). These include the Electronic Prescribing (eRx) Incentive Program, Medicare and Medicaid’s Electronic Health Records (EHR) Incentive Program, the Physician Quality Reporting System (PQRS), and the upcoming transition to ICD-10. This article will give a brief description of each of these programs and provide you with the information you need to take advantage of available incentives and avoid penalties by becoming compliant. Electronic Prescribing (eRx) Incentive Program The eRx Incentive program is designed to facilitate the transition to electronic prescribing software through incentive payments and penalties. E-prescribing can be achieved through standalone software or through Electronic Health Records that have an e-prescribing capability. The first year of the program that features both incentive payments and payment adjustments (penalties) is 2012. Eligible professionals who successfully reported eRx measures in 2011 received a 1 percent bonus payment from Medicare in 2012. In 2012, physicians must report the eRx measure for at least 25 unique electronic prescribing events in which the measure is reportable by the eligible professionals during 2012 in order to be eligible for the 1 percent incentive payment. Physicians who fail to report at least 25 prescribing events or report the G8553 code via claims for at least 10 unique denominator-eligible eRx events for services provided January 1, 2011, through June 30, 2011, will be subject to a 1 percent payment penalty for all Medicare payments in 2012. There is also a group practice reporting option (GRPO) that allows groups to earn a 1 percent incentive payment. Eligible professionals may be exempt from the application of the payment penalty if CMS determines that compliance with the requirement for being a successful electronic prescriber would result in a significant hardship. Applications for a hardship exemption are due by June 30, 2012. It is important to note that for each year physicians do not meet the criteria for successful electronic prescribing, payment penalties increase. In 2013, physicians may be subject to a 1.5-percent penalty, and in 2014 this increases to a 2-percent payment penalty. For more information on the eRx Incentive Program, see the Academy’s information page at http://www.entnet.org/Practice/MedicareERxFactSheet.cfm. Medicare and Medicaid’s Electronic Health Records (EHR) Incentive Program The Electronic Health Records Incentive Program is an initiative from CMS designed to facilitate the use of EHRs in clinical settings. Eligible professionals, hospitals, and critical access hospitals that demonstrate meaningful use of EHRs are eligible for incentive payments. Incentive payments can accumulate to up to $44,000 by 2015 if eligible professionals begin to successfully participate in 2012. The EHR Incentive Program is structured in three stages, with a possible fourth stage starting in 2018. In order to successfully demonstrate meaningful use in Stage 1, which began in 2011, eligible professionals must meet 20 objectives out of 25 possible choices. There are 15 required core objectives, while the remaining five objectives may be chosen from the list of 10 menu set objectives. Eligible professionals must report on six total clinical quality measures: three required core measures (substituting alternate core measures where necessary) and three additional measures (selected from 38 clinical quality measures). The meaningful use criteria for Stage 2, which is scheduled to begin in 2014, were proposed by CMS in early March and are expected to be finalized sometime in the summer of 2012. The Academy will provide timely updates on the development of Stage 2 meaningful use criteria. Just like the eRx program, there are coming penalties for professionals who do not begin participating in the EHR Incentive Program. Starting in 2015, eligible professionals, hospitals, and critical access hospitals that do not successfully demonstrate meaningful use of EHRs will be subject to a 1 percent penalty that increases annually up to 5 percent by 2020. For more information on the EHR Incentive Program, visit the Academy’s information page at http://www.entnet.org/Practice/ONC.cfm. Physician Quality Reporting System (PQRS) The Physician Quality Reporting System is currently a voluntary reporting program that provides an incentive payment to physicians or groups that report data on quality measures. In 2012, physicians who successfully report data on quality measures are eligible for .5 percent bonus payment on all Medicare claims. Individual eligible professionals may choose to report information on individual physician quality reporting quality measures or measures groups to CMS on their Medicare Part B claims, to a qualified Physician Quality Reporting registry, or to CMS via a qualified EHR product, or to a qualified Physician Quality Reporting data submission vendor. The Academy currently offers an online tool named PQRIwizard to help collect and report quality measure data for the PQRS program in 2012. PQRIwizard offers automatic data validation, minimized data entry time, and retrospective or prospective data submission. Information for PQRIwizard can be found at http://www.entnet.org/Practice/PQRS.cfm. Beginning in 2015, CMS will adopt a payment penalty as part of the PQRS program like the eRx and EHR programs. Eligible professionals who do not satisfactorily submit PQRS quality measure data face a 1.5 percent payment penalty. This penalty rises to 2 percent in 2016. To avoid the 2015 payment penalty, an eligible professional must satisfactorily report PQRS quality measure data during the 2013 reporting period (January 1, 2013, to December 21, 2013). For more information on PQRS, visit the Academy’s information page at http://www.entnet.org/Practice/cmsPQRIBonus.cfm. The Transition to International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) As the enforcement deadline for the transition to the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Version 5010 approaches, providers and billers must take heed of the fact that penalties for non-compliance could be severe. On April 1 the Office of E-Standards and Services began enforcement of any complaints it receives for non-compliance. Notably, providers can be penalized up to $1.5 million annually for uncorrected, repeated, willful neglect of compliance with new HIPAA standards. Although it may be unlikely that the Department of Health and Human Services (HHS) will exercise such extreme enforcement capabilities, the possibility exists. While HHS has announced intent to delay the ICD-10 compliance deadline of October 1, 2013, it did not delay the 5010 enforcement deadline. Further, providers should understand that part of the Electronic Health Record (EHR) Incentive Payment Program for 2012 consists of submitting all electronic claims under 5010. Even with the potential ICD-10 delay, your practice should work to become compliant with ICD-10 by October 1, 2013, (or by the time of implementation) to avoid delayed payments from Medicare and private payers. Although CMS has not created a specific penalty structure for non-compliance with ICD-10, providers will still fall under the same HIPAA umbrella of regulations and again may be fined up to $1.5 million for uncorrected willful neglect with a maximum of $50,000 per violation. The Academy originally opposed the ICD-10 transition and advocated for a delay in the compliance deadline in previous efforts, to help our members during the transition. For any questions or information about these programs, email the Health Policy unit at healthpolicy@entnet.org or visit the Regulatory and Socioeconomic Affairs site at http://www.entnet.org/Practice/ regulatorySocioAdvocacy.cfm. YEAR INCENTIVE (+) PENALTY (-) 2012 eRx +1% PQRS +0.5% eRx -1% 2013 PQRS +0.5% eRx -1.5% ICD-10 Implemntation (likely delayed) 2014 PQRS +0.5% eRx -2% 2015 None EHR -1% PQRS -1.5% 2016 None PQRS -2% 2020 None EHR -5% Incentives, Penalties Related to Technology: What You Should Be Aware Of, How the Academy Is Helping Members Note from the AAO-HNS/F President Rodney P. Lusk, MD Those of you who don’t think the incentive is worth the time and expense to adopt these new technologies, you need to beware that for many of the technology incentive programs mentioned in the 3P article by Richard W. Waguespack, MD, and Michael Setzen, MD, there will soon be penalties that can total as much as 10 percent from all Medicare payments for your practice. This adds up and may really affect you as the reimbursement for Medicare procedures continues to decline. The Academy takes every opportunity to meet with CMS and submit comments related to these various programs, their overlapping time frames, and potential for future penalties. In March, the Academy participated in an AMA sign-on letter that expressed concerns to CMS about the various quality program payment penalties, which are rapidly approaching and will affect providers all within a very narrow time frame. The Academy is diligently working on your behalf to help you with information about participating in these programs. There is a lot of helpful information on the Academy website and the Meaningful Use, EHR, and eRX pages have recently been updated. Take note of the important highlights below about the Physician Quality Reporting System (PQRS). PQRS: The Academy currently offers an online tool named the PQRIwizard to help collect and report quality measure data for the PQRS program. PQRIwizard was first made available for the 2011 reporting period and the tool is currently being revised for 2012. The PQRIwizard tool calculates your PQRS quality measures and includes a built-in progress monitor to validate your report. Unlike 2011, the 2012 edition of PQRIwizard will include a selection of individual measures specific to otolaryngology. The importance of participation in PQRS continues to grow as CMS will adopt a payment adjustment (penalty) in 2015 for physicians who do not satisfactorily submit PQRS quality measure data. To avoid the 2015 payment adjustment, physicians must satisfactorily report PQRS data during the 2013 reporting period. Information for the PQRIwizard can be found on the website at http://www.entnet.org/Practice/PQRS.cfm.
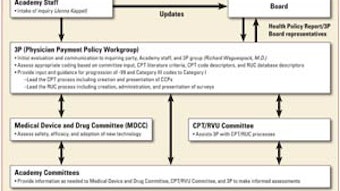
Richard W. Waguespack, MD, coordinator for Socioeconomic Affairs and Michael Setzen, MD, coordinator for Practice Affairs, Co-chairs of 3P Health Policy staff: Jean Brereton, senior director, Research, Quality, and Health Policy; Jenna Kappel, director, Health Policy; Jenna Minton, senior manager, Health Policy; Joe Cody, Health Policy analyst; Harrison Peery, Health Policy analyst
The Physician Payment Policy Workgroup (3P), co-chaired by Richard W. Waguespack, MD, and Michael Setzen, MD, is the senior advisory body to Academy leadership and staff on issues related to socioeconomic advocacy, regulatory activity, coding or reimbursement, and practice services or management. 3P and the Health Policy staff have been busy in 2012 with a continued high level of activity, constant emails, and monthly calls, working diligently and tirelessly on behalf of all members.
Below, we want to draw your attention to the fact that, in the next few years, there will be numerous opportunities through incentives and potential minefields by way of penalties that will affect your practice as technological advances change the way we practice medicine (see Table 1). These include the Electronic Prescribing (eRx) Incentive Program, Medicare and Medicaid’s Electronic Health Records (EHR) Incentive Program, the Physician Quality Reporting System (PQRS), and the upcoming transition to ICD-10. This article will give a brief description of each of these programs and provide you with the information you need to take advantage of available incentives and avoid penalties by becoming compliant.
Electronic Prescribing (eRx) Incentive Program
The eRx Incentive program is designed to facilitate the transition to electronic prescribing software through incentive payments and penalties. E-prescribing can be achieved through standalone software or through Electronic Health Records that have an e-prescribing capability. The first year of the program that features both incentive payments and payment adjustments (penalties) is 2012. Eligible professionals who successfully reported eRx measures in 2011 received a 1 percent bonus payment from Medicare in 2012.
In 2012, physicians must report the eRx measure for at least 25 unique electronic prescribing events in which the measure is reportable by the eligible professionals during 2012 in order to be eligible for the 1 percent incentive payment. Physicians who fail to report at least 25 prescribing events or report the G8553 code via claims for at least 10 unique denominator-eligible eRx events for services provided January 1, 2011, through June 30, 2011, will be subject to a 1 percent payment penalty for all Medicare payments in 2012. There is also a group practice reporting option (GRPO) that allows groups to earn a 1 percent incentive payment. Eligible professionals may be exempt from the application of the payment penalty if CMS determines that compliance with the requirement for being a successful electronic prescriber would result in a significant hardship. Applications for a hardship exemption are due by June 30, 2012.
It is important to note that for each year physicians do not meet the criteria for successful electronic prescribing, payment penalties increase. In 2013, physicians may be subject to a 1.5-percent penalty, and in 2014 this increases to a 2-percent payment penalty.
For more information on the eRx Incentive Program, see the Academy’s information page at http://www.entnet.org/Practice/MedicareERxFactSheet.cfm.
Medicare and Medicaid’s Electronic Health Records (EHR) Incentive Program
The Electronic Health Records Incentive Program is an initiative from CMS designed to facilitate the use of EHRs in clinical settings. Eligible professionals, hospitals, and critical access hospitals that demonstrate meaningful use of EHRs are eligible for incentive payments. Incentive payments can accumulate to up to $44,000 by 2015 if eligible professionals begin to successfully participate in 2012.
The EHR Incentive Program is structured in three stages, with a possible fourth stage starting in 2018. In order to successfully demonstrate meaningful use in Stage 1, which began in 2011, eligible professionals must meet 20 objectives out of 25 possible choices. There are 15 required core objectives, while the remaining five objectives may be chosen from the list of 10 menu set objectives. Eligible professionals must report on six total clinical quality measures: three required core measures (substituting alternate core measures where necessary) and three additional measures (selected from 38 clinical quality measures). The meaningful use criteria for Stage 2, which is scheduled to begin in 2014, were proposed by CMS in early March and are expected to be finalized sometime in the summer of 2012. The Academy will provide timely updates on the development of Stage 2 meaningful use criteria.
Just like the eRx program, there are coming penalties for professionals who do not begin participating in the EHR Incentive Program. Starting in 2015, eligible professionals, hospitals, and critical access hospitals that do not successfully demonstrate meaningful use of EHRs will be subject to a 1 percent penalty that increases annually up to 5 percent by 2020.
For more information on the EHR Incentive Program, visit the Academy’s information page at http://www.entnet.org/Practice/ONC.cfm.
Physician Quality Reporting System (PQRS)
The Physician Quality Reporting System is currently a voluntary reporting program that provides an incentive payment to physicians or groups that report data on quality measures. In 2012, physicians who successfully report data on quality measures are eligible for .5 percent bonus payment on all Medicare claims. Individual eligible professionals may choose to report information on individual physician quality reporting quality measures or measures groups to CMS on their Medicare Part B claims, to a qualified Physician Quality Reporting registry, or to CMS via a qualified EHR product, or to a qualified Physician Quality Reporting data submission vendor.
The Academy currently offers an online tool named PQRIwizard to help collect and report quality measure data for the PQRS program in 2012. PQRIwizard offers automatic data validation, minimized data entry time, and retrospective or prospective data submission. Information for PQRIwizard can be found at http://www.entnet.org/Practice/PQRS.cfm.
Beginning in 2015, CMS will adopt a payment penalty as part of the PQRS program like the eRx and EHR programs. Eligible professionals who do not satisfactorily submit PQRS quality measure data face a 1.5 percent payment penalty. This penalty rises to 2 percent in 2016. To avoid the 2015 payment penalty, an eligible professional must satisfactorily report PQRS quality measure data during the 2013 reporting period (January 1, 2013, to December 21, 2013).
For more information on PQRS, visit the Academy’s information page at http://www.entnet.org/Practice/cmsPQRIBonus.cfm.
The Transition to International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10)
As the enforcement deadline for the transition to the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Version 5010 approaches, providers and billers must take heed of the fact that penalties for non-compliance could be severe. On April 1 the Office of E-Standards and Services began enforcement of any complaints it receives for non-compliance. Notably, providers can be penalized up to $1.5 million annually for uncorrected, repeated, willful neglect of compliance with new HIPAA standards. Although it may be unlikely that the Department of Health and Human Services (HHS) will exercise such extreme enforcement capabilities, the possibility exists. While HHS has announced intent to delay the ICD-10 compliance deadline of October 1, 2013, it did not delay the 5010 enforcement deadline. Further, providers should understand that part of the Electronic Health Record (EHR) Incentive Payment Program for 2012 consists of submitting all electronic claims under 5010.
Even with the potential ICD-10 delay, your practice should work to become compliant with ICD-10 by October 1, 2013, (or by the time of implementation) to avoid delayed payments from Medicare and private payers. Although CMS has not created a specific penalty structure for non-compliance with ICD-10, providers will still fall under the same HIPAA umbrella of regulations and again may be fined up to $1.5 million for uncorrected willful neglect with a maximum of $50,000 per violation. The Academy originally opposed the ICD-10 transition and advocated for a delay in the compliance deadline in previous efforts, to help our members during the transition.
For any questions or information about these programs, email the Health Policy unit at healthpolicy@entnet.org or visit the Regulatory and Socioeconomic Affairs site at http://www.entnet.org/Practice/ regulatorySocioAdvocacy.cfm.
| YEAR | INCENTIVE (+) | PENALTY (-) |
|---|---|---|
| 2012 | eRx +1% PQRS +0.5% |
eRx -1% |
| 2013 | PQRS +0.5% | eRx -1.5% ICD-10 Implemntation (likely delayed) |
| 2014 | PQRS +0.5% | eRx -2% |
| 2015 | None | EHR -1% PQRS -1.5% |
| 2016 | None | PQRS -2% |
| 2020 | None | EHR -5% |
Incentives, Penalties Related to Technology: What You Should Be Aware Of, How the Academy Is Helping Members
Note from the AAO-HNS/F President Rodney P. Lusk, MD
Those of you who don’t think the incentive is worth the time and expense to adopt these new technologies, you need to beware that for many of the technology incentive programs mentioned in the 3P article by Richard W. Waguespack, MD, and Michael Setzen, MD, there will soon be penalties that can total as much as 10 percent from all Medicare payments for your practice. This adds up and may really affect you as the reimbursement for Medicare procedures continues to decline.
The Academy takes every opportunity to meet with CMS and submit comments related to these various programs, their overlapping time frames, and potential for future penalties. In March, the Academy participated in an AMA sign-on letter that expressed concerns to CMS about the various quality program payment penalties, which are rapidly approaching and will affect providers all within a very narrow time frame.
The Academy is diligently working on your behalf to help you with information about participating in these programs. There is a lot of helpful information on the Academy website and the Meaningful Use, EHR, and eRX pages have recently been updated. Take note of the important highlights below about the Physician Quality Reporting System (PQRS).
PQRS: The Academy currently offers an online tool named the PQRIwizard to help collect and report quality measure data for the PQRS program. PQRIwizard was first made available for the 2011 reporting period and the tool is currently being revised for 2012. The PQRIwizard tool calculates your PQRS quality measures and includes a built-in progress monitor to validate your report. Unlike 2011, the 2012 edition of PQRIwizard will include a selection of individual measures specific to otolaryngology. The importance of participation in PQRS continues to grow as CMS will adopt a payment adjustment (penalty) in 2015 for physicians who do not satisfactorily submit PQRS quality measure data. To avoid the 2015 payment adjustment, physicians must satisfactorily report PQRS data during the 2013 reporting period. Information for the PQRIwizard can be found on the website at http://www.entnet.org/Practice/PQRS.cfm.