OUT OF COMMITTEE: PATIENT SAFETY AND QUALITY IMPROVEMENT: Transforming OR performance with post-op debrief tracking
In an effort to mitigate human error and optimize efficiency and quality, patient safety checklists have been incorporated in managing the operating room suite. The preoperative surgical time-out mandated and outlined by The Joint Commission (TJC) has been extensively studied and is now considered the standard of care.
By: Carol M. Lewis, MD, MPH, and Alex J. McKinlay, MD

In an effort to mitigate human error and optimize efficiency and quality, patient safety checklists have been incorporated in managing the operating room suite. The preoperative surgical time-out mandated and outlined by The Joint Commission (TJC) has been extensively studied and is now considered the standard of care. The World Health Organization (WHO), TJC, the Association of periOperative Registered Nurses, and the Agency for Healthcare Research and Quality (AHRQ) also advocate a postoperative debriefing to be done after the procedure and before the patient leaves the operating room. In fact, this has been a part of the WHO’s Surgical Safety Checklist since 2008.1 AHRQ recommends debriefing after any clinical event as a learning strategy to promote reflection, identify problems, and direct improvement initiatives. 2
Debriefing has its roots in military performance improvement tools, implemented in World War II when soldiers returning from missions were questioned.3 It made its way into healthcare through medical simulation programs, where debriefing methods were formalized.2 Debriefing allows for the identification and discussion of failures and near failures as well as successes, and serves as a method of experiential learning. It improves interdisciplinary communication and, by identifying and addressing errors and best practices, performance improvement. Postoperative debriefing has been associated with improved error identification and team communication and collaboration as well as procedure-specific improvements.3 In a study by Bandari, et al., 54 percent of 6,000 operating room safety hazards were identified during the debriefing process.4 Other survey-based studies highlight the benefits of improved teamwork, collegiality, and professionalism—particularly in the realms of “participative safety” and “vision.”5,6
Detractors tend to voice logistical and efficiency-related concerns, citing the additional time it adds to operating room protocol and the potential of delaying turnover. However, a study of more than 37,000 cases found that a debriefing tool took only an average of 2.5 minutes to complete.7 Arguably, the improved efficiency resulting from debriefings offsets this time cost. Importantly, the debrief reinforces and sustains the institutional culture of safety.
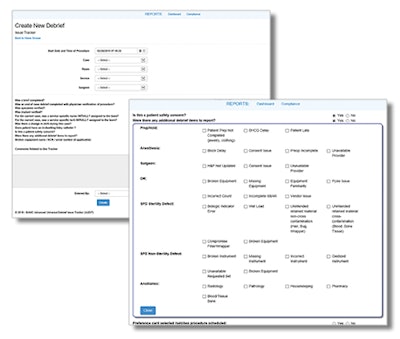 Figure 1: Sample debriefing
Figure 1: Sample debriefing
Studies indicate the potential power of such information; one study used debriefing to identify areas for improvement in cases of obstetric hemorrhage, resulting in a 33 percent decrease in massive transfusions and a 78 percent decrease in unplanned hysterectomies.8 The authors emphasized that debriefing is critical for identifying areas of improvement as well as, but determining if recommended interventions are actually used in clinical practice.
To better collect and analyze the data from debriefs, a variety of software debrief tracking tools have been developed. Debrief trackers can be customized for any given institution’s resources and needs and can be quite comprehensive. It is helpful to collect data on delays (and their duration), issues with OR equipment, instrument sets, ancillary services such as radiology, pathology, and pharmacy, and the timeliness of all employees and providers participating in the operating room.
An example of one debrief tracker utilized at a large tertiary care referral center and level 1 trauma center is displayed in Figure 1, designed by otolaryngologist Jessica J. Kepchar, DO.
By systematically and routinely collecting intraoperative data on every case in the operating room via a debrief tracker, the organization becomes equipped with informative data. Dashboards can then display the data to a full spectrum of interested participants, from the end users to management. Such data bring new perspective to operating room-related problem solving. It becomes simple to identify trends. Why are cases starting late? Why do certain services struggle with longer turnovers? Why are intra-operative imaging services so inefficient? A close look at the dashboard primes leaders to find the answers. Continued use of the trackers elicits additional organizational benefits: transparency and accountability. Research even supports a link between these principles and lower mortality rates.9
One of the author’s institutions developed a debrief tracker in response to a challenge with sterile processing and distribution (SPD) service. It quickly became evident that a reliable, single source of intra-operative data would be invaluable in shaping our collective way to improvement. It took months of iterative changes in deciding which data we would collect and how we would collect it to ultimately reach an effective tool.
Key learning points for us included simplifying the data collection process to facilitate minable data—dichotomous and objective whenever possible, clearly assigning specific roles to specific OR personnel (for example who is responsible for starting and leading the debrief, who is responsible for electronically recording the data of the debrief, etc.), conducting deliberate training and marketing campaigns throughout the hospital for awareness, and following up with auditing and re-training efforts.
Each of these proved critical. Equipped with the tracker and an intuitive dashboard, the otolaryngology service began to analyze otolaryngology-specific data. We quickly ascertained that we had a few specific issues with our tympanomastoidectomy sets and fixed them just as quickly.
Our collaborative improvement efforts with SPD were clearly facilitated by the data that both parties had at our fingertips. In addition, clinical leaders in the otolaryngology department continued to use debrief tracker data to trend patterns (late starts, delays, etc.), solve problems, and recognize performance (on-time starts, efficient turnovers, etc.).
Although not as widely adopted as the pre-operative time-out, postoperative debriefing is as equally vital to the success of perioperative communication and process improvement. Appropriately developed and maintained, an effective debriefing process, such as a codified debrief tracking software, is a game-changing tool in shaping patient safety and process in the operating room.
References
- Haynes AB, Weiser TG, Berry WR, et al. A Surgical Safety Checklist to Reduce Morbidity and Mortality in a Global Population. NEJM. 2009;360:491-499.
- Debriefing for Clinical Learning. Agency for Healthcare Research and Quality: Patient Safety Network. https://psnet.ahrq.gov/primers/primer/36/Debriefing-for-Clinical-Learning. Last updated 1/2019. Accessed 6/6/2019.
- Zuckerman AL, France DJ, Green C, et al. Surgical debriefing: a reliable roadmap to completing the patient safety cycle. Neurosurg Focus. 2012;33:1-8.
- Bandari J, Schumacher K, Simon M, et al. Surfacing safety hazards using standardized operating room briefings and debriefings at a large regional medical center. Jt Comm J Qual Patient Saf. 2012;38:154-160.
- Papaspyros SC, Javangula KC, Adluri RK, et al. Briefing and debriefing in the cardiac operating room: analysis of impact on the theatre team attitude and patient safety. Interact Cardiovasc Thorac Surg. 2010;10:43-47.
- Leong KBMSL, Hanskamp-Sebregts M, van der Wal RA, et al. Effects of perioperative briefing and debriefing on patient safety: a prospective intervention study. BMJ Open. 2017;7:e018367.
- Berenholtz SM, Schumacher K, Hayanga AJ, et al. Implementing standardized operating room briefings and debriefings at a large regional medical center. Jt Comm J Qual Patient Saf. 2009;35:391-397.
- Corbett N, Hurko P, Vallee JT. Debriefing as a Strategic Tool for Performance Improvement. J Obstet Gynecol Neonatal Nurs. 2012;41:572-579.
- Toffolutti V, Stuckler D. A Culture of Openness Is Associated With Lower Mortality Rates Among 137 English National health Service Acute Trusts. Health Aff (Millwood). 2019 May;38(5):844-850.