The Art of Tonsillectomy: The UK Experience for the Past 100 Years
Napoleon Charaklias, MRCS, DOHNS, MSc; Constantinos Mamais, MRCS, DOHNS, MCh; B. Nirmal Kumar, MBBS, MPhil, DLO, FRCS (ORL-HNS) Tonsillectomy is one of the oldest operations in surgery. Celsus in De Medicina (47 BC) gives the earliest description of tonsillectomy. Various descriptions exist in the world’s literature dating from Galen and Paul of Aegina to Ambrose Paré. George Ernest Waugh is the father of tonsillectomy, as it is known today. In 1909, he pioneered the subcapsular blunt dissection and reported no complications in more than 700 patients. An alternative method of “cold steel” tonsillectomy is the guillotine technique, where the tonsil is amputated using a specially designed guillotine device. Otto Oswald Popper introduced the haemostatic guillotine in 1929. The introduction of various instruments has greatly facilitated tonsillectomy. In 1948, Sir Victor Negus introduced curved forceps and the knot pusher. The Boyle-Davis gag (Dr. Henry Edmund Gaskin Boyle was a pioneer anesthetist) was designed for use with tracheal tubes to improve surgical access to the oropharynx. Initially, the anesthetic team had to hold it in position while the surgeon operated. David Alexander Draffin’s idea was to suspend it on a bipod consisting of two rods dedicated “to the weary hands of cooperative anesthetists and nurses.” A key event in the history of tonsillectomy was the National Prospective Tonsillectomy Audit in 2005. It was the biggest audit conducted in the UK, involving 250 institutions and more than 40,000 patients. After a review of practice and complication rates in the first 28 days, hot techniques, such as electrocautery or coblation tonsillectomy, were shown to be associated with double the complication rates compared with cold techniques (table 1). The ‘‘cold steel” technique, as performed 100 years ago, is still associated with fewer complication rates than new techniques. In the last 100 years, we have failed to agree to an optimal technique for tonsillectomy. Maybe in the next 100? Technique % postoperative hemorrhage % return to theatre Cold steel dissection with ties and packs 1.30 1.0 Cold steel dissection with diathermy haemostasis 2.9 1.7 Bipolar scissors 3.9 2.4 Monopolar diathermy 6.1 4.0 Coblation 4.4 3.1 Subcapsular blunt dissection pioneered by Dr. Waugh. This article is based on a paper presented September 12, 2011, during the Otolaryngology Historical Society meeting. If you are interested in presenting at the 2012 OHS meeting on September 10 in Washington, DC, or wish to join or renew as an OHS member, email museum@entnet.org. References Waugh GE. A simple operation for the complete removal of tonsils, with notes on 900 cases. Lancet. 1909;1:1314-1315. Draffin DA. A useful bipod. Br Med J. 1951;2:52-53. ENT Comparative Audit Group and RCS (Eng.) Clinical Effectiveness Unit National Prospective Tonsillectomy Audit: Final Report. London: The Royal College of Surgeons; 2005. http://www.entuk.org/members/audits/tonsil/Tonsillectomyauditreport_Pdf. – See more at: http://aaobulletin.365.staging2.ascendmedia.com/Highlight.aspx?id=4570&p=392#sthash.poZfIRWK.dpuf
Napoleon Charaklias, MRCS, DOHNS, MSc; Constantinos Mamais, MRCS, DOHNS, MCh; B. Nirmal Kumar, MBBS, MPhil, DLO, FRCS (ORL-HNS)
 George Ernest Waugh, father of modern tonsillectomy.
George Ernest Waugh, father of modern tonsillectomy.Tonsillectomy is one of the oldest operations in surgery. Celsus in De Medicina (47 BC) gives the earliest description of tonsillectomy. Various descriptions exist in the world’s literature dating from Galen and Paul of Aegina to Ambrose Paré.
George Ernest Waugh is the father of tonsillectomy, as it is known today. In 1909, he pioneered the subcapsular blunt dissection and reported no complications in more than 700 patients.
An alternative method of “cold steel” tonsillectomy is the guillotine technique, where the tonsil is amputated using a specially designed guillotine device. Otto Oswald Popper introduced the haemostatic guillotine in 1929.
The introduction of various instruments has greatly facilitated tonsillectomy. In 1948, Sir Victor Negus introduced curved forceps and the knot pusher.
The Boyle-Davis gag (Dr. Henry Edmund Gaskin Boyle was a pioneer anesthetist) was designed for use with tracheal tubes to improve surgical access to the oropharynx. Initially, the anesthetic team had to hold it in position while the surgeon operated. David Alexander Draffin’s idea was to suspend it on a bipod consisting of two rods dedicated “to the weary hands of cooperative anesthetists and nurses.”
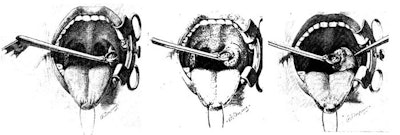
 Boyle-Davis mouth gag, Draffin rod, and the Negus curved forceps and knot pusher.
Boyle-Davis mouth gag, Draffin rod, and the Negus curved forceps and knot pusher.A key event in the history of tonsillectomy was the National Prospective Tonsillectomy Audit in 2005. It was the biggest audit conducted in the UK, involving 250 institutions and more than 40,000 patients. After a review of practice and complication rates in the first 28 days, hot techniques, such as electrocautery or coblation tonsillectomy, were shown to be associated with double the complication rates compared with cold techniques (table 1).
The ‘‘cold steel” technique, as performed 100 years ago, is still associated with fewer complication rates than new techniques. In the last 100 years, we have failed to agree to an optimal technique for tonsillectomy. Maybe in the next 100?
| Technique | % postoperative hemorrhage | % return to theatre |
|---|---|---|
| Cold steel dissection with ties and packs | 1.30 | 1.0 |
| Cold steel dissection with diathermy haemostasis | 2.9 | 1.7 |
| Bipolar scissors | 3.9 | 2.4 |
| Monopolar diathermy | 6.1 | 4.0 |
| Coblation | 4.4 | 3.1 |
 |
||
| Subcapsular blunt dissection pioneered by Dr. Waugh. |
This article is based on a paper presented September 12, 2011, during the Otolaryngology Historical Society meeting. If you are interested in presenting at the 2012 OHS meeting on September 10 in Washington, DC, or wish to join or renew as an OHS member, email museum@entnet.org.
References
Waugh GE. A simple operation for the complete removal of tonsils, with notes on 900 cases. Lancet. 1909;1:1314-1315.
Draffin DA. A useful bipod. Br Med J. 1951;2:52-53.
ENT Comparative Audit Group and RCS (Eng.) Clinical Effectiveness Unit National Prospective Tonsillectomy Audit: Final Report. London: The Royal College of Surgeons; 2005. http://www.entuk.org/members/audits/tonsil/Tonsillectomyauditreport_Pdf.
– See more at: http://aaobulletin.365.staging2.ascendmedia.com/Highlight.aspx?id=4570&p=392#sthash.poZfIRWK.dpuf








