The path to healthcare reform
Last month, I raised the premise that meaningful healthcare reform could not be accomplished without the participation and cooperation of all participants in the debate.
 James C. Denneny III, MD
James C. Denneny III, MD
AAO-HNS/F EVP/CEO
Many would say that the U.S. population is the most over-medicated and over-treated in the world. The constant bombardment of promising solutions to every problem has created hopes of perfection that can’t be achieved. This has triggered a frenzy of consumption that has been unjustified by results achieved. Unless there is a reorientation to the incremental value of additional services, we cannot provide basic services to all who need them.
It is time to define a goal of what we need to provide for the public and work backward to get there. Neither a single-payer system, nor a hybrid of the system we currently have can support the current cost structure, even when limited to essential benefits. The out-of-pocket expenses that currently exist are unmanageable for most of our population. All in the group of 11 contribute to this problem. Perfection has become the enemy of good and will preclude success moving forward.
The current tort system—not just malpractice, but also product liability—sets the tone for progressive and often unjustified regulatory add-ons that contribute little but cost to the system. The current system has not been shown to significantly modify behavior as claimed by its proponents. There have been some improvements at the state level relating to malpractice, but the even more costly product liability needs to be handled at the federal level.
As will be required by several existing conditions, Congress will need to overcome significant lobbies to benefit the whole. I think we are all tired of seeing the plethora of advertisements imploring those who have used some product to call that particular law firm to “get the compensation you deserve.” Additionally, the direct-to-consumer pharmaceutical ads touting unconscionably expensive products with often marginal benefit over existing products create artificial demand from unwary consumers.
An army of consultants advises the healthcare industry, particularly hospital systems and medical device companies, on how to maximize profits, often circumventing well-intended policies. The added layers of “middlemen” and bureaucracy have inflated costs beyond belief. It should be no surprise that costs have escalated when we recognize that since 1990, the Bureau of Labor Statistics records a >3,000 percent increase in healthcare administrators compared to just over a 100 percent increase in physicians.
Rules affecting “non-profits” have served to accelerate the “arms race” we are seeing in hospital systems’ building programs across the country. Do these palatial structures actually improve care and results?
Ancillary services are overpromoted, overpriced, and often not necessary in many circumstances. The health insurance industry seemed very happy to support these extravagant costs in an inconsistent fashion while adding their 20+ percent margin to the pot.
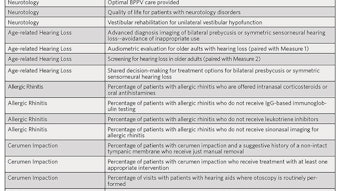
While the majority of physicians want the best for their patients, a meaningful minority have become distracted by opportunities primarily designed to increase revenue. Medicine is in the process of defining quality, “value,” and best care, but we are still a considerable way from achieving that goal. In the meantime, we must do a better job of policing ourselves and promoting appropriate care.
Should these 11 groups fail to recognize the urgency of the overall situation and refuse to compromise on these basic issues, at best they risk an extreme regulatory environment and at worst, a crash of the system. One segment cannot be asked to bear the entire burden of change, and we already know that the alternating “band-aid” approach has failed at virtually every turn. How do we get a group such as this to convene, knowing that they will each need to make meaningful sacrifices to reach a successful conclusion? Prior to convening a definitive convention, the first step is an honest, introspective look at current resource utilization by each group and identification of systemic changes that can be combined with those of other groups toward the goal of overall cost reduction.