CY 2018 Medicare physician fee schedule (MPFS): What does it mean for you?
On July 13, 2017, the Centers for Medicare & Medicaid Services (CMS) posted the proposed rule for payments in the Medicare Physician Fee Schedule (MPFS) for calendar year (CY) 2018.

On July 13, 2017, the Centers for Medicare & Medicaid Services (CMS) posted the proposed rule for payments in the Medicare Physician Fee Schedule (MPFS) for calendar year (CY) 2018. The Academy submitted comments to CMS on the proposed rule on September 1, 2017. Some key provisions members should be aware of from the proposed rule include:
Conversion factor
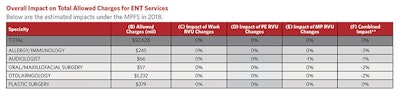
CMS estimates a CY 2018 conversion factor of $35.9903, which reflects the 0.5 percent update specified by the Medicare Access and CHIP Reauthorization Act (MACRA), a budget neutrality adjustment, and a target recapture amount mandated by the Protecting Access to Medicare Act of 2014 (PAMA). Overall, this is a slight increase from the 2017 conversion factor of $35.8887.
Valuation of specific codes
The ABLE Act specifies that for services that are not new or revised codes, if the total RVUs for a service for a year would otherwise be decreased by an estimated 20 percent or more as compared to the total RVUs for the previous year, the applicable adjustments in work, PE, and MP RVUs shall be phased-in over a two-year period. Otolaryngology had three services on this list for CY 2018:
- Muscle Flaps (CPT codes 15732, 15736, 15738, 157X1, and 157X2): CPT codes 15732 and 15736 were identified via a screen of high level E/M visits included in their global periods. This screen identified that a CPT code 99214 office visit was included for CPT codes 15732 and 15736 but not included in the other codes in this family. During the review process for this family of codes, CPT code 15732 was deleted and replaced with two new codes, CPT codes 157X1 and 157X2, to better differentiate and describe the work of large muscle flaps performed on patients with head and neck cancer depending on the site where the service was performed.
For CY 2018, CMS proposes the RUC-recommended work RVUs for CPT codes 15734 (a work RVU of 23.00), 15736 (a work RVU of 17.04), 15738 (a work RVU of 19.04), 157X1 (a work RVU of 13.50), and 157X2 (a work RVU of 15.68). - Resection Inferior Turbinate (CPT code 30140): CPT code 30140 was identified as potentially misvalued on a screen of Harvard-valued codes with utilization over 30,000 in CY 2014. During the review process, the RUC resurveyed the code as a 0-day global period, based on the presence of a negative intensity value in the initial survey and highly variable postoperative office visits. For CY 2018, CMS proposes the RUC-recommended work RVU of 3.00 for CPT code 30140 as a 0-day global code.
CMS also proposes to create equipment codes for three new equipment items based on invoices submitted with the RUC recommendations for CPT code 30140: the 2mm reusable shaver blade (EQ383) at a price of $790, the microdebrider handpiece (EQ384) at a price of $4,760, and the microdebrider console (EQ385) at a price of $9,034. - Control Nasal Hemorrhage (CPT codes 30901, 30903, 30905, and 30906): For CY 2018, CMS proposes the RUC-recommended work RVUs for CPT codes 30901 (a work RVU of 1.10), 30903 (a work RVU of 1.54), 30905 (a work RVU of 1.97), and 30906 (a work RVU of 2.45). It also proposes to use the RUC-recommended direct PE inputs for CPT codes 30901, 30903, 30905, and 30906, with standard refinements to the equipment times to account for patient monitoring times.
- Nasal Sinus Endoscopy (CPT codes 31254, 31255, 31256, 31267, 31276, 31287, 31288, 31295, 31296, 31297, 31XX1, 31XX2, 31XX3, 31XX4, and 31XX5): In October 2016, the CPT Editorial Panel created five new codes (CPT codes 31XX1, 31XX2, 31XX3, 31XX4 and 31XX5) and revised CPT codes 31238, 31254, 31255, 31276, 31287, 31288, 31296, and 31297. CPT codes 31XX2 – 31XX5 are newly bundled services representing services that are frequently reported together, and CPT code 31XX1 represents a new service. The RUC reviewed this family of codes at their January 2017 meeting. The ESS and BSD codes were selected for review when they triggered CMS screening parameters, based on the performance of certain combinations of these codes more than 75 percent of the time. The significance of the revaluation of these commonly performed procedures led the Academy to partner with the American Rhinologic Society (ARS) and the American Academy of Otolaryngic Allergy (AAOA) to convene a panel of experts to submit recommendations and solicit physician survey participants. This task force worked for more than a year to create the combined codes and prepare for the RUC valuation process, and its consensus recommendations were critical to the presentation of these codes at the RUC meeting. The survey results demonstrated a significant decrease in reported intraservice for respondents to complete each procedure. This was particularly significant in the ESS codes, which had not been previously surveyed since the early 1990s. These drops in intraservice time resulted in decreased values for the ESS codes, ranging from -7.9 percent to -23.6 percent. The BSD codes, which had been surveyed in 2011, were more consistent with the previous values. For CY 2018, CMS proposes the RUC-recommended work RVUs for all 15 CPT codes in this family, specifically existing and newly-developed Endoscopic Sinus Surgery (ESS) and balloon sinus dilation (BSD) codes.
- Tracheostomy (CPT codes 31600, 31601, 31603, 31605, and 31610): CPT code 31600 was identified as part of a screen of high expenditure services with Medicare- allowed charges of $10 million or more that had not been recently reviewed. CPT codes 31601, 31603, 31605, and 31610 were added and reviewed as part of the code family. CMS is proposing the RUC-recommended work RVUs for all five codes in this family.
- Percutaneous Allergy Skin Tests (CPT code 95004): In the CY 2016 PFS proposed rule (80 FR 41706), CPT code 95004 was identified through the high expenditures screen as potentially misvalued. The RUC and CMS previously determined that there is physician work involved in providing this service since the physician must interpret the test and prepare a report. For CY 2018, CMS is proposing the RUC-recommended work RVU of 0.01 for CPT code 95004. Regarding direct PE inputs, CMS is proposing to refine the equipment times for exam table (EF023) and mayo stand (EF015) to 79 minutes each to account for clinical 1:4 patient monitoring time. CMS received invoices with new pricing information for two supplies: SH101 “negative control, allergy test” ($5.17) and SH102 “positive control, allergy test” ($26.12). Using this information, CMS is proposing a price of $0.03 per test for supply item SH101 and a price of $0.13 per test for supply item SH102.
Appropriate Use Criteria (AUC) for advanced diagnostic imaging
In the CY 2018 proposed rule, CMS proposes that ordering professionals must consult specified applicable Appropriate Use Criteria (AUC) through qualified clinical decision support mechanisms (CDSMs) for applicable imaging services furnished in an applicable setting, paid for under an applicable payment system, and ordered on or after January 1, 2019. This comes after CMS identified the circumstances specific to ordering professionals under which consulting and reporting requirements are not required. Additionally, in the CY 2017 fee schedule final rule, CMS published the first list of clinical areas to guide identification for outlier ordering professionals. CMS did not identify mechanisms for consultation by April 1, 2016, and therefore did not require ordering professionals to consult CDSMs or furnishing professionals to report information on the consultation by the January 1, 2017, date.
CMS also states that payment may only be made if the order includes (1) which qualified CDSM was consulted by the ordering professional; (2) whether the service ordered would adhere to specified applicable AUC, would not adhere to specified applicable AUC, or whether specified applicable AUC were not applicable to the service ordered; and (3) the NPI of the ordering professional (if different from the furnishing professional). This standard would apply across all applicable payment systems and across claim types. To implement this requirement, CMS proposes establishing a series of G-codes to describe the specific CDSM that was used by the ordering professional. CMS intends for there to be one G-code for every qualified CDSM with the code description including the name of the CDSM.
For 2018, CMS proposes keeping the following AUC program significant hardship exceptions identified in the 2017 final rule: Insufficient Internet Connectivity; Extreme and Uncontrollable Circumstances; Lack of Control over the Availability of CEHRT; and Lack of Face-to-Face Patient Interaction. For CY 2018, CMS also proposes an exemption for ordering professionals who are granted reweighting of the advancing care information (ACI) performance category to zero percent of the final MIPS score for the year. Lastly, CMS proposes to give Merit-based Incentive Program (MIPS) credit to ordering professionals for consulting AUC using a qualified CDSM as a high-weight improvement activity for the performance period beginning January 1, 2018.
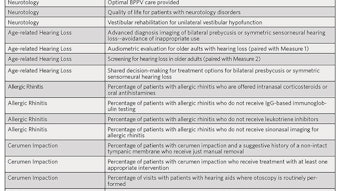
PQRS and CQMs
Under the proposed rule, CMS proposes to modify the criteria for data already submitted for the CY 2016 reporting period to determine whether an individual eligible professional (EP) or group practice has satisfactorily reported for purposes of avoiding the 2018 PQRS payment adjustment. CMS proposes to revise the previously finalized satisfactory reporting criteria for the CY 2016 reporting period to lower the requirement from nine measures across three NQS domains, where applicable, to only six measures with no domain or cross-cutting measure requirement.
Value-based payment modifier and physician feedback program
Due to the changes in reporting, for the CY 2018 adjustment period, CMS proposes reducing the automatic downward adjustment for groups with 10 or more EPs and at least one physician to -2 percent, and -1 percent for groups with between two to nine EPs, physician solo practitioners, and for groups and solo practitioners that consist only of non-physician EPs. CMS also proposes to hold all groups and solo practitioners that avoid a PQRS payment adjustment harmless and reduce the maximum upward adjustment under the quality-tiering methodology to two times an adjustment factor (+2.0x) for groups with 10 or more EPs.
To read more on the fee schedule or review the detailed member summary, you may visit the Academy’s Regulatory Advocacy page at: http://www.entnet.org/content/regulatory-advocacy.