Speaking up for physician well-being
The American Council for Graduate Medical Education (ACGME) recently released recommendations related to the 80-hour work week for resident trainees.
 James C. Denneny III, MD
James C. Denneny III, MD
AAO-HNS/F EVP/CEO
It is no secret that daily the practice of medicine, as well as that of other healthcare professions, is becoming more complex and stressful. A “healthy” workforce is critical to optimizing care for patients. “Physician burnout” has far-reaching implications in the United States healthcare delivery system. Medical errors have been shown to increase significantly and patient satisfaction decline substantially as the burnout phenomenon increases. While physician well-being is not a new topic, it has expanded greatly since the “resident syndrome” was recognized in the 1970s. Currently, it is estimated that greater than 60 percent of the physician workforce experiences burnout. This is more than two times the rate of the general population and is increasing persistently. The resultant depression, substance abuse, and suicides are reaching crisis proportions, and clearly the situation will require the collaborative intervention of all stakeholders in healthcare delivery.
I recently participated in the National Academy of Medicine (NAM) Action Collaborative on Clinician Well-Being and Resilience in Washington, DC. Participants included representatives from medical associations, the nursing community, the ACGME, the Accreditation Council for Continuing Medical Education (ACCME), government and private payers, the American Hospital Association, the Federation of State Medical Boards, the American Board of Medical Specialties, the National Patient Safety Foundation, the Agency for Healthcare Research and Quality (AHRQ), large healthcare systems, and the Surgeon General of the United States. This group has committed to work together to heighten awareness of the serious nature of this issue as well as identify and modify both internal and external factors that combine to worsen the current situation.
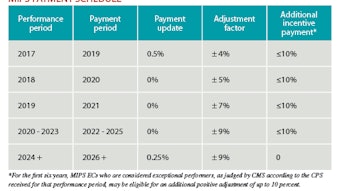
This process will require a commitment of resources from all stakeholders to identify, research, and catalog the underlying systemic and individual components responsible for creating the current state of affairs regarding clinician well-being. A number of significant systemic issues face providers today led by a plethora of electronic health records concerns but also including healthcare delivery system changes, payment changes, and the expanding excess of regulatory requirements, with more alterations expected under the new Administration. There is also the formidable task of changing the “culture” that physicians and nurses navigate currently. This culture of self-neglect and denial only tends to perpetuate and intensify the problem. The Academy looks forward to working with this collaborative effort led by the NAM to improve the lives of our Members through changes to the system and educational efforts to positively affect the day-to-day practice of medicine.
World Voice Day (April 16) materials are available at http://www.entnet.org/WorldVoiceDay. It is time to extend the reach of the message, “share your voice,” and highlight the crisis healthcare providers are facing today.
International programs
Your president, Gregory W. Randolph, MD, has been leading our efforts along with our distinguished international team to operationalize the ongoing upgrade to our international programs being rolled out at our AAO-HNSF 2017 Annual Meeting & OTO Experience in Chicago. Considerable time and effort are being spent to ensure the successful launch of our International Advisory Board (IAB) this fall in Chicago. The inaugural chair and vice-chair of the IAB, Johan Fagan, MD, and Sady Selaimen da Costa, MD, PhD, are actively involved with Academy leadership including Dr. Randolph and the international coordinator, James E. Saunders, MD, and coordinator-elect, J. Pablo Stolovitzky, MD, in formulating the goals and operational parameters for the IAB. We will offer CME at the International Symposium under the direction of Mark K. Wax, MD, at the Annual Meeting, and we continue to expand our education portfolio for distribution to otolaryngologists worldwide.