Academy toolkit for MIPS reporting in 2017
The Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 created the Quality Payment Program (QPP), containing two pathways for participation: the Merit-based Incentive Payment System (MIPS) and the Advanced Alternative Payment Model (APM) program.
2017 MIPS participation requirements
All physicians, physician assistants, nurse practitioners, clinical nurse specialists, or certified registered nurse anesthetists who bill Medicare must participate in MIPS, unless they:
- Have not previously participated in Medicare
- If 2017 is a clinician’s first year participating in Medicare, then the clinician is not required to report to MIPS for the 2017 reporting period.
- Do not meet the minimum reporting threshold
- ECs who bill Medicare for $30,000 or less in allowed Medicare charges OR see 100 or fewer Medicare Part B patients for a year are excluded from MIPS reporting for that year.
- Are part of an Advanced APM
- ECs who receive 25 percent of Medicare payments or see 20 percent of their Medicare patients through an Advanced APM in 2017 are excluded from MIPS reporting for that year.
Reg-ent and 2017 MIPS participation
Reg-ent is an otolaryngology-specific clinical data registry, through which participants will be able to report the required MIPS categories, including Quality Measures, Advancing Care Information Measures, and Improvement Activities. Sign up by July 15, 2017, to make Reg-ent your MIPS reporting partner! Learn more about Reg-ent here: www.entnet.org/reg-ent.
Important dates for MIPS
During the 2017 MIPS performance period, there are several key dates and deadlines for ECs and groups:
- January 1, 2017: The first performance period opens.
- July 15, 2017: Reg-ent enrollment deadline to report MIPS 2017.
- October 2, 2017: To be eligible for the maximum positive payment adjustment in 2019, ECs must begin MIPS reporting before this date.
- December 31, 2017: The first performance period closes.
- March 31, 2018: ECs must submit their 2017 performance data by this date.
- January 1, 2019: The payment adjustments based on 2017 will go into effect by this date.
Please Note: In the 2017 performance period, Cost does not count toward an EC’s final MIPS CPS and will not affect 2019 payments. In the 2018 performance period, CMS will begin using the Cost category to determine EC payment adjustment.
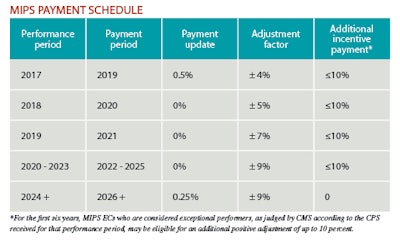
MIPS payment update schedule
When MACRA replaced the SGR and created MIPS, MACRA legislated the payment update schedule, adjustment factor, and additional incentive payments available to ECs. For the MIPS payment schedule set by MACRA, please see the table.
Additional information
Want more information? The Academy has created a wealth of resources, including specific reporting requirements for each of the performance score categories, available online through the Academy’s MIPS page and MIPS brochure. The MIPS page is available here: www.entnet.org/content/mips. Access the AAO-HNS/F MIPS brochure here: www.entnet.org/mips-reporting.











