Joint Commission: Meaningful change?
The expanding list of rules governing how one practices medicine both in the hospital and outpatient setting has been recognized as one of the greatest threats to physician well-being in the medical community today.
James C. Denneny III, MD
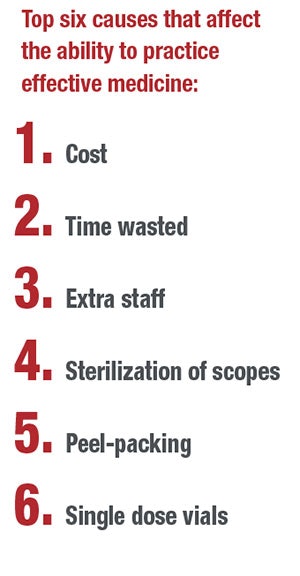
The expanding list of rules governing how one practices medicine both in the hospital and outpatient setting has been recognized as one of the greatest threats to physician well-being in the medical community today. Whether it’s the EHR, documentation requirements irrelevant to best patient care, operating room attire, sterilization requirements, or “peel-packing” of outpatient office instruments, the frustration and anger is palpable. The cost of compliance in terms of financial resources in addition to physician and staff time is high and sometimes prohibitive at a time when both have exceeded rational limits. When you include the toll that these burdens take on physician resiliency and wellness, it is easy to understand the reaction we are seeing now.
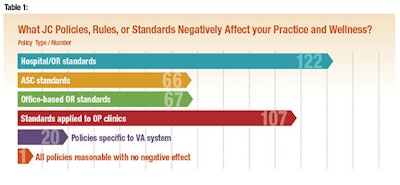
As part of an updated strategy to present our concerns to the Joint Commission (JC), a survey was sent out this spring through ENTConnect and OTO News. We had a robust response of 158 members who contributed to the survey results. We asked six questions, including three that required a detailed response. All practice types were represented with 39.2 percent designated as private practice, 33.5 percent as academic, 18.4 percent as employed by hospital systems, and 8.9 percent representing military practices. When asked “What JC policies negatively affect your practice and wellness,” the respondents’ top answer was “Hospital/OR policies.” (See Table 1.)
— C.W. David Chang, MD
AAO-HNSF Co-Chair, PSQI Committee
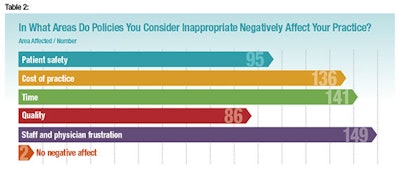
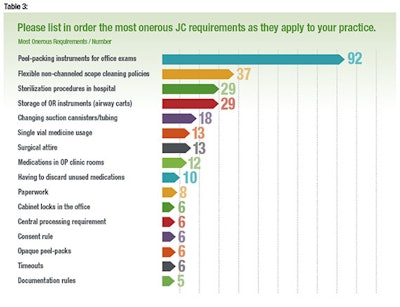
The most common negative effect of JC policies was staff and physician frustration. (See Table 2.) When asked to list the most onerous policies as they affect the respondent’s practice, peel-packing office instruments was the Number One concern. (See Table 3.) It was difficult to accurately estimate monetary costs for the different practice settings, but the majority of respondents agreed it was over $10,000 per physician per year.
Some of the more notable quotations from respondents included:
- “People wonder what happened to the ‘old time physicians’ … I think that a lot of empathy, generosity, and kindness has gotten beaten out of them … glad you asked.”
- “The fact that I need to spend time on this survey is symbolic of how there are so many restrictions that serve no evidence-based positive patient care purpose, yet are inconvenient and wasteful of my time and money.”
- “I could not begin to convince the JAHCO surveyor that this was a solution to a non-existent problem.”
- “I cannot estimate the cost. One avoidable death is too many.”
There is a great need to pursue policy that is meaningful in terms of results through evidence-based data as well as that allows an efficient, cost-effective practice of medicine. We are working to establish foundations that allow both goals to be met.















