(How) Can We Influence Our Future? Part II
Presenting the otolaryngologist’s indispensable role in providing the best patient care is essential in ensuring that our members are given appropriate responsibility and their patients have access to care for their medical needs.
 James C. Denneny III, MD
James C. Denneny III, MD
AAO-HNS/F Executive Vice President and CEO
- Evidential needs that can be validated as “difference makers” for patient care
- How the specialty can and must come together in this effort
- How we can identify additional allies and partners to help push this across the finish line with advocacy excellence
Best Care for Patients
Physicians, otolaryngologists in our case, should be the ones defining what is the “best care” for the areas that we are the clinical experts through well-designed, data-validated outcomes research. These outcome measures should be welcomed by all payers including the government, private insurance companies, or other interested parties as the critical element needed to develop a more cost-effective, value-based healthcare delivery system. Conceptually, technological advances and the widespread use of electronic health record systems in healthcare facilities and physician’s offices should create an ideal platform to gather the comprehensive depth and breadth of data that can be used to identify and define the “best care” for disease processes as well as the capability of delivering “personalized care” based on an individual’s likelihood of response to a proposed treatment.
However, the promise of the ability to collect all the data needed to successfully fuel the evidence machine that will optimize our ability to offer the most effective treatment based on a patient’s unique combination of environmental, genetic, and social factors has not been fulfilled. The potential to access this trove of information has been severely limited by the failure to establish and enforce data interoperability standards across the healthcare delivery landscape, despite repeated efforts by the medical and scientific community to secure a system that allows ready communication using a standardized operating system. Such a standard has existed for decades in the telecommunications industry, which allowed multiple competing companies to offer service to the population through a common network. This led to greater innovation within the industry as well.
The American Academy of Otolaryngology–Head and Neck Surgery and its Foundation (AAO-HNSF) Boards of Directors authorized the creation of the clinical data registry, Reg-entSM, to serve as a tool to gather the data related to the clinical practice of medicine that is necessary to investigate and define the character parameters mentioned above. Reg-ent was designed to also function as a resource in other areas as it matured and developed the capabilities to create value in the spaces critical to participating in the evolving healthcare delivery system. The figure below illustrates the multiple functions that Reg-ent can serve.
 Figure 1. Multiple functions of Reg-ENT.
Figure 1. Multiple functions of Reg-ENT.
Reg-ent has been a reliable avenue for MIPS reporting since its inception and is prepared to continue that role as long as Medicare participation requires reporting to avoid penalties to the already inadequate physician payment system. Our Reg-ent team has been instrumental in developing a new pathway, MIPS Value Pathways (MVP), for the next iteration of the MIPS reporting. The data needed to report on the existing Medicare quality measures reflects only a portion of that required to determine outcomes, conduct clinical research, and participate in pharmaceutical and device trials.
It has been considerably more difficult to gather nonstructured and ancillary data than was initially projected. Progress has been slower than anticipated, largely due to the failure of the industry to adopt a single standard. Our Reg-ent team is currently looking at different strategies and technologies that will allow us to fully capture the data we need to facilitate meaningful analytic projects. This is an area where artificial intelligence (AI) brings significant value in accessing and understanding the nonstructured data fields that are so critical to including all elements in the end product. The complete clinical data set can then be enhanced through multiple other data sources that can add mortality, payer, pharmacy, and utilization data to give a full picture of each area of study. Our analytic partner, OM1, brings the ability to add these, as well as other data sources, to our clinical data in addition to normalizing the data to prepare it for the desired research projects.
In addition to fully operationalizing our clinical data registry, we are also involved in identifying and pursuing vehicles that our members can use as the payment system transitions to a “value-based model.” We have been actively discussing a variation of our MVP proposal based on care pathways that can hopefully be converted into an alternate payment model with Medicare that would be considered to meet value-based goals. The ability to participate in such a model for Medicare patients has been elusive for specialty physicians, with no approved option available yet.
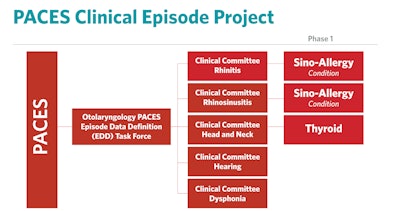
The private payer market is extremely interested in developing value-based payment models, and we are currently involved in a project with the Patient-Centered Episodes System (PACES) Center for Value in Healthcare Inc., a nonprofit organization that is seeking to develop an alternative payment model that groups health insurance claims into “episodes of care.” This system would also result in price and quality transparency and provide a reproducible, fair methodology to evaluate provider performance. Willard C. Harrill, MD, is leading this process to develop “episodes of care” models for five clinical areas as seen below. The AAO-HNSF has previously worked with the American College of Surgeons on a project like this several years ago focused on thyroid disease.
We firmly believe that evidence (data) will determine not only “best care” but will guide regulatory and private payer policy in the evolving healthcare payment system to value.
Specialty Unity
I have described the different approaches that our organization is engaged in to ensure that our members have every opportunity to be meaningful participants in the evolving healthcare delivery system, whichever direction it finally takes. To make this a reality, it will be essential that the specialty in the United States is able to speak with a unified voice that includes the full breadth of our subspecialty societies and the full spectrum of otolaryngology practice settings and special interest groups within otolaryngology-head and neck surgery. Any influence that our small specialty has will be dependent on a unified message that will benefit the whole of otolaryngology and their patients.
Enlisting Allies for Advocacy Excellence
The ability to enlist allies and partners within the house of medicine, including specialists, primary care, allied health providers, healthcare insurers, hospital systems, employers, and patient groups, will be crucial to achieving a meaningful long-term solution. Collaboration and agreement within these groups will be dependent on a transparent, evidence-supported plan that can be understood and is conceptually fair to all.
Even if otolaryngology is successful in all these areas that I have highlighted, including demonstrating and maintaining the foundational excellence needed to be the leaders in providing clinical healthcare in our areas of expertise, formulating creative strategies and models to address adequate access to care and services, creating “best care” paradigms through validated evidence, standing together as a specialty and with the house of medicine, and establishing meaningful partnerships across the healthcare landscape, we will not be successful without the right communication and advocacy excellence needed to inform the decision-makers and public of our strengths and plans.
Presenting the value of the otolaryngologist’s contributions to the healthcare system and indispensable role in providing the best patient care is essential in ensuring that our members are given appropriate responsibility and their patients have access to care for their medical needs must be done through advocacy excellence.
Our message must be transmitted effectively to both federal and state legislative bodies, the Administration’s regulatory bodies, and the participants in the private segment of the healthcare delivery system since each of these components will have considerable influence in developing novel solutions to improve our current system.
The most effective strategy for communicating our message to the various targets listed above involves consistency, early engagement, and member involvement. Once a platform is decided upon that the specialty can support, it is critical that all discussions focus on a consistent message that can be delivered in a variety of ways by our Academy’s Advocacy team and more importantly otolaryngologists around the country. The more physician participants that we can mobilize to individually deliver the message, the stronger our voice and the higher likelihood of success.
We will need to energize our advocacy networks through the Board of Governors and specialty societies to be ready to promote solutions for problems and lead the push for a better system. Those who care about the conditions and rules they will practice under during their careers as physicians need to personally engage as part of our Advocacy team. It is incumbent on the Academy to create the platform to support and educate our member volunteers who will be leading this fight.