Clinical Practice Guideline: Evaluation of neck mass in adults
The primary purpose of the Clinical Practice Guideline: Evaluation of the Neck Mass in Adults is to promote the efficient, effective, and accurate diagnostic work-up of neck masses to ensure that adults with potentially malignant disease receive prompt diagnosis and intervention to optimize outcomes.

The primary purpose of the Clinical Practice Guideline: Evaluation of the Neck Mass in Adults is to promote the efficient, effective, and accurate diagnostic work-up of neck masses to ensure that adults with potentially malignant disease receive prompt diagnosis and intervention to optimize outcomes. This guideline does not apply to children. Instead, this guideline is restricted to addressing the appropriate work-up of an adult patient with a neck mass that may be malignant in order to expedite diagnosis and referral to a head and neck cancer specialist.
The 2017 guideline was chaired by Melissa A. Pynnonen, MD, with M. Boyd Gillespie, MD, MSc, and Benjamin R. Roman, MD, MSHP, serving as assistant chairs, and Richard M. Rosenfeld, MD, MPH, as the methodologist, and David E. Tunkel, MD, as methodologist-in-training.
The guideline is endorsed to date by American Academy of Physician Assistants, American Academy of Emergency Medicine, American Association of Oral and Maxillofacial Surgeons, American College of Radiology, American Head and Neck Society, American Society for Clinical Pathology, Head and Neck Cancer Alliance, Society of Otorhinolaryngology Head-Neck Nurses, and Triological Society.
The full guideline, as well as other resources, is available at http://www.entnet.org/content/clinical-practice-guideline-evaluation-neck-mass-adults and in Otolaryngology–Head and Neck Surgery as published at www.otojournal.org.
The target patient for this guideline is 18 years or older with a neck mass. The target clinician for this guideline is the first clinician a patient with a neck mass encounters. This includes clinicians in primary care, dentistry, and emergency medicine, as well as pathologists and radiologists who have a role in diagnosing neck mass.
Guideline key action statements
1. Avoidance of antibiotic therapy
Clinicians should not routinely prescribe antibiotic therapy for patients with a neck mass unless there are signs and symptoms of bacterial infection.
2a. Stand-alone suspicious history
Clinicians should identify patients with a neck mass who are at increased risk for malignancy because the patient lacks a history of infectious etiology and the mass has been present for two weeks or greater without significant fluctuation or the mass is of uncertain duration.
2b. Standalone suspicious physical examination
Clinicians should identify patients with a neck mass who are at increased risk for malignancy based on one or more of these physical examination characteristics: fixation to adjacent tissues, firm consistency, size greater than 1.5 cm, and/or ulceration of overlying skin.
2c. Additional suspicious signs and symptoms
Clinicians should conduct an initial history and physical examination for all adults with a neck mass to identify those patients with other suspicious findings that represent an increased risk for malignancy.
3. Follow-up of the patient not at increased risk
For patients with a neck mass who are not at increased risk for malignancy, clinicians or the designees should advise patients of criteria that would trigger the need for additional evaluation. Clinicians or their designees should also document a plan for followup to assess resolution or final diagnosis.
4. Patient education
For patients with a neck mass who are deemed at increased risk for malignancy, clinicians or their designees should explain to the patient the significance of being at increased risk and explain any recommended diagnostic tests.
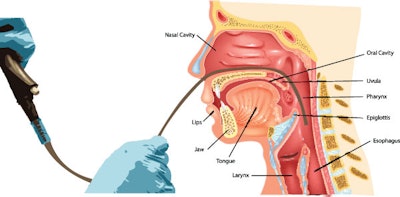
5. Targeted physical examination
Clinicians should perform, or refer the patient to a clinician who can perform, a targeted physical examination (including visualizing the mucosa of the larynx, base of tongue, and pharynx), for patients with a neck mass deemed at increased risk for malignancy.
6. Imaging
Clinicians should order a neck computed tomography (or magnetic resonance imaging) with contrast for patients with a neck mass deemed at increased risk for malignancy.
7. Fine needle aspiration (FNA)
Clinicians should perform FNA instead of open biopsy, or refer the patient to someone who can perform FNA, for patients with a neck mass deemed at increased risk for malignancy when the diagnosis of the neck mass remains uncertain.
8. Cystic masses
For patients with a neck mass deemed at increased risk for malignancy, clinicians should continue evaluation of patients with a cystic neck mass, as determined by FNA or imaging studies, until a diagnosis is obtained and should not assume the mass is benign.
9. Ancillary tests
Clinician should obtain additional ancillary tests based on the patient’s history and physical examination when a patient with a neck mass is at increased risk for malignancy and/or does not have a diagnosis after FNA and imaging.
10. Examination under anesthesia of the upper aerodigestive tract before open biopsy
Clinicians should recommend examination of the upper aerodigestive tract under anesthesia, before open biopsy, for patients with a neck mass who are at increased risk for malignancy and without a diagnosis or primary site identified, with FNA, imaging, and/or ancillary tests.
AAO-HNSF Guideline development process and the obligations associated with the guideline recommendations are documented in the Clinical Practice Guideline Development Manual, Third Edition: a quality-driven approach for translating evidence into action. (http://oto.sagepub.com/content/148/1_suppl/S1.long)
Guideline authors
Melissa A. Pynnonen, MD (Chair), M. Boyd Gillespie, MD, MSc (Assistant Chair), Benjamin R. Roman, MD, MSHP (Assistant Chair), Richard M. Rosenfeld, MD, MPH (Methodologist), David E. Tunkel, MD (Methodologist-in-Training), Laura Bontempo, MD, MEd, Itzhak Brook, MD, MSc, Davoren Ann Chick, MD, Maria Colandrea, DNP, NP-C, CORLN, CCRN, Sandra A. Finestone, PsyD, Jason C. Fowler, PA-C, Christopher C. Griffith, MD, Zeb Henson, MD, Corinna Levine, MD, MPH, Vikas Mehta, MD, Andrew Salama, DDS, MD, Joseph Scharpf, MD, Deborah R. Shatzkes, MD, Wendy B. Stern, MD, Jay S. Youngerman, MD
Disclaimer
The clinical practice guideline is provided for information and educational purposes only. It is not intended as a sole source of guidance in evaluating neck masses. Rather, it is designed to assist clinicians by providing an evidence-based framework for decision-making strategies. The guideline is not intended to replace clinical judgment or establish a protocol for all individuals with this condition and may not provide the only appropriate approach to diagnosing and managing this program of care. As medical knowledge expands and technology advances, clinical indicators and guidelines are promoted as conditional and provisional proposals of what is recommended under specific conditions but are not absolute. Guidelines are not mandates; these do not and should not purport to be a legal standard of care. The responsible physician, in light of all circumstances presented by the individual patient, must determine the appropriate treatment. Adherence to these guidelines will not ensure successful patient outcomes in every situation. The AAO-HNSF emphasizes that these clinical guidelines should not be deemed to include all proper treatment decisions or methods of care, or to exclude other treatment decisions or methods of care reasonably directed to obtaining the same results.
See the Patient Information Fact Sheets:
Adult Neck Mass Follow-up
Frequently Asked Questions for Adults with a Neck Mass
Examination Under Anesthesia: What Should the Adult Patient Expect?
Neck Mass Biopsy: What Should the Adult Patient Expect?