Updated Clinical Practice Guideline: Otitis Media with Effusion
New evidence, systematic reviews, randomized control trials, and an evolved methodology that includes consumers necessitated an update to “Clinical Practice Guideline: Otitis Media with Effusion,” released this month as a supplement to Otolaryngology–Head and Neck Surgery.

New evidence, systematic reviews, randomized control trials, and an evolved methodology that includes consumers necessitated an update to “Clinical Practice Guideline: Otitis Media with Effusion,” released this month as a supplement to Otolaryngology–Head and Neck Surgery. The update, already endorsed by the American Academy of Family Physicians (AAFP), replaces the 2004 guideline co-developed by the AAO-HNSF, the AAFP, and the American Academy of Pediatrics (AAP).
Richard M. Rosenfeld, MD, MPH, chaired both the 2004 guideline and the 2016 update.
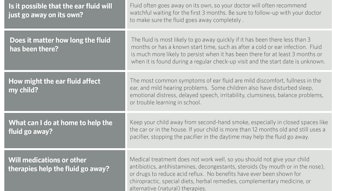
“You really could call OME an occupational hazard of early childhood,” said Dr. Rosenfeld. “Given its prevalence—most kids will experience it by the time they are school age—we emphasize materials in this update that will help doctors better communicate with parents and caregivers. There are new teaching aids, frequently asked questions, and grids to aid in shared decision-making.”
Other differences between the 2004 guideline and the 2016 update include:
- additional information on pneumatic otoscopy and tympanometry to improve diagnostic certainty;
- expanded information on speech and language assessment for children with otitis media with effusion (OME);
- new recommendations for managing OME in children who fail a newborn hearing screen and for evaluating at-risk children;
- a new recommendation against using topical intranasal steroids;
- a new recommendation against adenoidectomy for a primary indication of OME in children under 4 years of age;
- a new recommendation for assessing OME outcomes.
“Physicians will notice that each statement in the guideline explicitly links with a quality improvement opportunity, and we’ve included an algorithm flow chart that links all the statements together in a cohesive and understandable way,” Dr. Rosenfeld said.
The full guideline, as well as other resources, is available at www.entnet.org/OMECPG as well as in Otolaryngology–Head and Neck Surgery as published at otojournal.org.
Guideline recommendations
Pneumatic otoscopy (a)
The clinician should document the presence of middle ear effusion with pneumatic otoscopy when diagnosing OME in a child.
Pneumatic otoscopy (b)
The clinician should perform pneumatic otoscopy to assess for OME in a child with otalgia, hearing loss, or both.
Tympanometry
Clinicians should obtain tympanometry in children with suspected OME for whom the diagnosis is uncertain after performing (or attempting) pneumatic otoscopy.
Failed newborn hearing screen
Clinicians should document in the medical record counseling of parents of infants with OME who fail a newborn hearing screen regarding the importance of follow-up to ensure that hearing is normal when OME resolves and to exclude an underlying sensorineural hearing loss (SNHL).
Identifying at-risk children
Clinicians should determine if a child with OME is at increased risk for speech, language, or learning problems from middle ear effusion because of baseline sensory, physical, cognitive, or behavioral factors.
Evaluating at-risk children
Clinicians should evaluate at-risk children for OME at the time of diagnosis of an at-risk condition and at 12 to 18 months of age (if diagnosed as being at-risk prior to this time).
Screening healthy children
Clinicians should not routinely screen children for OME who are not at-risk and do not have symptoms that may be attributable to OME, such as hearing difficulties, balance (vestibular) problems, poor school performance, behavioral problems, or ear discomfort.
Patient education
Clinicians should educate families of children with OME regarding the natural history of OME, need for follow-up, and the possible sequelae.
Watchful waiting
Clinicians should manage the child with OME who is not at-risk with watchful waiting for three months from the date of effusion onset (if known) or three months from the date of diagnosis (if onset is unknown).
Steroids
Clinicians should recommend against using intranasal steroids or systemic steroids for treating OME.
Antibiotics
Clinicians should recommend against using systemic antibiotics for treating OME.
Antihistamines or decongestants
Clinicians should recommend against using antihistamines, decongestants, or both for treating OME.
Hearing test
Clinicians should obtain an age-appropriate hearing test if OME persists for three months or longer OR for OME of any duration in an at-risk child.
Speech and language
Clinicians should counsel families of children with bilateral OME and documented hearing loss about the potential impact on speech and language development.
Surveillance of chronic OME
Clinicians should reevaluate, at three- to six-month intervals, children with chronic OME until the effusion is no longer present, significant hearing loss is identified, or structural abnormalities of the eardrum or middle ear are suspected.
Surgery for children less than 4 years old
Clinicians should recommend tympanostomy tubes when surgery is performed for OME in a child less than 4 years old; adenoidectomy should not be performed unless a distinct indication (e.g., nasal obstruction, chronic adenoiditis) exists other than OME.
Surgery for children age 4 years old or older
Clinicians should recommend tympanostomy tubes, adenoidectomy, or both when surgery is performed for OME in a child 4 years old or older.
Outcome assessment
When managing a child with OME clinicians should document in the medical record resolution of OME, improved hearing, or improved quality of life (QOL).
Guideline authors
Richard M. Rosenfeld, MD, MPH; Jennifer J. Shin, MD, SM; Seth R. Schwartz, MD, MPH; Robyn Coggins, MFA; Lisa Gagnon, MSN, CPNP; Jesse M. Hackell, MD; David Hoelting, MD; Lisa L. Hunter, PhD, FAAA; Ann W. Kummer, PhD, CCC-SLP; Spencer C. Payne, MD; Dennis S. Poe, MD, PhD; Maria Veling, MD; Peter M. Vila, MD, MSPH; Sandra A. Walsh, and Maureen D. Corrigan.
Disclaimer
The clinical practice guideline is provided for information and educational purposes only. It is not intended as a sole source of guidance in managing OME. Rather, it is designed to assist clinicians by providing an evidence-based framework for decision-making strategies. The guideline is not intended to replace clinical judgment or establish a protocol for all individuals with this condition and may not provide the only appropriate approach to diagnosing and managing this program of care. As medical knowledge expands and technology advances, clinical indicators and guidelines are promoted as conditional and provisional proposals of what is recommended under specific conditions but are not absolute. Guidelines are not mandates; these do not and should not purport to be a legal standard of care. The responsible provider, in light of all circumstances presented by the individual patient, must determine the appropriate treatment. Adherence to these guidelines will not ensure successful patient outcomes in every situation. The AAO-HNSF emphasizes that these clinical guidelines should not be deemed to include all proper treatment decisions or methods of care, or to exclude other treatment decisions or methods of care reasonably directed to obtaining the same results.