The SGR bill passes: Advocacy does work
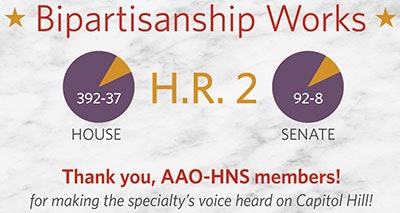
By James C. Denneny III, MD, AAO-HNS/F EVP/CEO The recent passage of H.R. 2, the Medicare Access and CHIP Reauthorization Act (MACRA), by Congress signaled the end of a 14-year journey that included 17 short-term “patches” for Medicare’s flawed Sustainable Growth Rate (SGR) physician payment formula that was enacted in 1997. Not only did this landmark bipartisan bill address the yearly threat of significant decreases in Medicare physician payments, it also: Consolidated the quality reporting requirements for Medicare providers. Beginning in 2019, the Merit-Based Incentive Payment System (MIPS) will consolidate existing quality programs and focus on quality, resource use, meaningful use, and clinical practice improvement in a cohesive fashion. The quality measures chosen by CMS utilized by Qualified Clinical Data Registries (QCDR) will be automatically included. In addition, federal funding will be available to help physicians develop additional quality measures from 2015-2019. Halted the CMS-mandated conversion away from 10- and 90-day global packages to 0-day billing parameters. Pursuant to the provisions of H.R. 2, CMS is required to gather data related to the recommended changes to the global packages by the end of 2017, prior to initiation of any new policy. Established positive payment updates for five years. A .5 percent increase in Medicare physician payments will help provide stability as physicians transition to the new system. Incentivized participation in an Alternative Payment Model (APM). Physicians who partake in various APMs will receive a 5 percent bonus from 2019-2024. During the debate, it was both amazing and rewarding to listen to both Democrat and Republican legislators articulate the same arguments that organized medicine had been putting forward for more than a decade as to why this proposal needed to be passed. The critical bipartisan interaction between Speaker of the U.S. House of Representatives, John Boehner, and the House Minority Leader, Nancy Pelosi, is an excellent example of how meaningful legislation can be passed when a spirit of compromise exists. Following their lead, the U.S. Senate and President Obama passed and signed the bill respectively. Overall, 484 legislators supported H.R. 2 – a rare demonstration of bipartisanship in the volatile political environment on Capitol Hill. Why did this happen? The physician community had a unified message. What was different in 2014 and 2015 compared to previous years? For one, the price tag to repeal and replace the flawed SGR formula was the lowest it had been in some time. Also, an effective Congressional Doctors’ Caucus partnered with Committee leaders and the physician community to broker the historic compromise in early 2014. Despite the disappointment of not passing the bill last year, the physician community and its dedicated members persisted in bringing forth the rational arguments that eventually resulted in passage of this bill in April 2015. This was not an accident, but a result of years of work by multiple physician groups, including the AAO-HNS, to educate Members of Congress on the issues and the consequences of inaction. Personal relationships built and nurtured over many years, along with the consistency and appeal of the message, put this effort over the top. Tens of thousands of physicians, along with their staffs, persisted with the same compelling message, despite year after year of failure to achieve permanent repeal. Members of Congress kept hearing the same message through advocacy outreach and grassroots efforts. These included Capitol Hill visits, political fundraisers, phone calls, emails, and tweets – all with the same message. This culminated in the passage of this landmark legislation and the subsequent signing into law by President Obama. Our message was heard. I would like to salute our legislative advocacy team headed by Joy Trimmer, JD, and thank all of you who contacted their personal representatives and senators. The same strategy of building relationships and establishing trust while advocating for the best patient care has also demonstrated success in dealing with both CMS and private payers. Collaborative efforts within otolaryngology have recently been fruitful as demonstrated by the reversal of the ruling by CMS concerning implantable hearing devices ( AAO-HNS, ANS, AOS), acceptance of group reporting measures by CMS (AAO-HNS, ABOto), and United Healthcare’s reversal of its policy that stated balloon ostial dilatation was experimental (AAO-HNS, ARS). In today’s regulatory environment, and now with the implementation of H.R. 2, there is some concern among our Members about the ability for private practitioners, particularly those in small group practices, to participate in these quality-based programs, which on the surface seem quite complex. The Academy’s commitment to build an otolaryngology-specific Qualified Clinical Data Registry (QCDR) by 2016 will allow direct reporting of pertinent measures by participants to CMS, as well as provide additional quality and payment benefits to our Members. We feel this tool will allow otolaryngologists to continue to practice successfully in a variety of practice settings. With SGR repeal finally a reality, what’s next? The AAO-HNS will continue to work to advance our specialty’s legislative priorities (liability reform, truth in advertising, patient safety/scope of practice, GME funding, etc.), minimize the increasing regulatory burdens on our members, and address private payer concerns such as network tiering, bundling of procedures, and payment denials. With your help and perseverance, we will continue to engage in all efforts to give our members the tools to provide the best care for their patients.
By James C. Denneny III, MD, AAO-HNS/F EVP/CEO
- Consolidated the quality reporting requirements for Medicare providers. Beginning in 2019, the Merit-Based Incentive Payment System (MIPS) will consolidate existing quality programs and focus on quality, resource use, meaningful use, and clinical practice improvement in a cohesive fashion. The quality measures chosen by CMS utilized by Qualified Clinical Data Registries (QCDR) will be automatically included. In addition, federal funding will be available to help physicians develop additional quality measures from 2015-2019.
- Halted the CMS-mandated conversion away from 10- and 90-day global packages to 0-day billing parameters. Pursuant to the provisions of H.R. 2, CMS is required to gather data related to the recommended changes to the global packages by the end of 2017, prior to initiation of any new policy.
- Established positive payment updates for five years. A .5 percent increase in Medicare physician payments will help provide stability as physicians transition to the new system.
- Incentivized participation in an Alternative Payment Model (APM). Physicians who partake in various APMs will receive a 5 percent bonus from 2019-2024.
Why did this happen? The physician community had a unified message. What was different in 2014 and 2015 compared to previous years? For one, the price tag to repeal and replace the flawed SGR formula was the lowest it had been in some time. Also, an effective Congressional Doctors’ Caucus partnered with Committee leaders and the physician community to broker the historic compromise in early 2014. Despite the disappointment of not passing the bill last year, the physician community and its dedicated members persisted in bringing forth the rational arguments that eventually resulted in passage of this bill in April 2015. This was not an accident, but a result of years of work by multiple physician groups, including the AAO-HNS, to educate Members of Congress on the issues and the consequences of inaction. Personal relationships built and nurtured over many years, along with the consistency and appeal of the message, put this effort over the top.
Tens of thousands of physicians, along with their staffs, persisted with the same compelling message, despite year after year of failure to achieve permanent repeal. Members of Congress kept hearing the same message through advocacy outreach and grassroots efforts. These included Capitol Hill visits, political fundraisers, phone calls, emails, and tweets – all with the same message. This culminated in the passage of this landmark legislation and the subsequent signing into law by President Obama. Our message was heard. I would like to salute our legislative advocacy team headed by Joy Trimmer, JD, and thank all of you who contacted their personal representatives and senators.
The same strategy of building relationships and establishing trust while advocating for the best patient care has also demonstrated success in dealing with both CMS and private payers. Collaborative efforts within otolaryngology have recently been fruitful as demonstrated by the reversal of the ruling by CMS concerning implantable hearing devices ( AAO-HNS, ANS, AOS), acceptance of group reporting measures by CMS (AAO-HNS, ABOto), and United Healthcare’s reversal of its policy that stated balloon ostial dilatation was experimental (AAO-HNS, ARS).
In today’s regulatory environment, and now with the implementation of H.R. 2, there is some concern among our Members about the ability for private practitioners, particularly those in small group practices, to participate in these quality-based programs, which on the surface seem quite complex. The Academy’s commitment to build an otolaryngology-specific Qualified Clinical Data Registry (QCDR) by 2016 will allow direct reporting of pertinent measures by participants to CMS, as well as provide additional quality and payment benefits to our Members. We feel this tool will allow otolaryngologists to continue to practice successfully in a variety of practice settings.
With SGR repeal finally a reality, what’s next? The AAO-HNS will continue to work to advance our specialty’s legislative priorities (liability reform, truth in advertising, patient safety/scope of practice, GME funding, etc.), minimize the increasing regulatory burdens on our members, and address private payer concerns such as network tiering, bundling of procedures, and payment denials. With your help and perseverance, we will continue to engage in all efforts to give our members the tools to provide the best care for their patients.











