CMS Proposes to Exclude Coverage of Osseointegrated Implants
Background On July 11, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule focusing on payment policy updates to the 2015 Durable Medical Equipment, Orthotics, Prosthetics and Supplies (DMEPOS) fee schedule. Notably, as part of the rule, CMS is proposing to clarify the scope of the Medicare coverage exclusion for hearing aids and withdraw coverage of all types of air conduction and bone conduction auditory prosthetics (external, internal, or implanted). If finalized, the proposed rule would negate CMS’current coverage of osseointegrated implants. CMS had expanded coverage to include osseointegrated implants as recently as 2005. In 2005, the auditory osseointegrated device was determined to be a new device category according to the new requirements for transitional pass-through payment during CMS’rulemaking. In the same regulatory revision, CMS additionally expanded coverage to both auditory osseointegrated devices and auditory brainstem devices, classifying them as prosthetic devices. In the past, CMS has traditionally addressed the scope of the Medicare hearing aid coverage exclusion through program instructions and national coverage policies or determinations. However, this year, CMS decided to clarify the definition and its coverage determination of a hearing aid in its proposed rulemaking and comment period for DMEPOS payment rates. CMS’ Rationale for its Proposed Coverage Exclusion In the proposed rule, CMS states that bone conduction auditory prosthetics (along with other devices classified as “hearing aids”) do not meet the statutory definition of a prosthetic device found at section 1861(s)(8) of the Social Security Act which, in part, states a “prosthetic devices (other than dental) which replace all or part of an internal body organ.”CMS also states that osseointegrated implants are, “bone conduction hearing aids that mechanically stimulate the cochlea; therefore, we believe that the hearing aid exclusion applies to these devices and propose that Medicare should not cover these devices, consistent with our interpretation of section 1862(a)(7) of the Act.”CMS additionally mentions in the rule that a National Coverage Determination (NCD) was issued for cochlear implant devices with, “…the result that this determination and recent requests to expand coverage of hearing devices raises serious questions about the intent and scope of the Medicare coverage exclusion for hearing aids.”CMS also claims it initiated its examination of its definition of a hearing aid after receiving multiple benefit category determination requests in recent years for the consideration of non-implanted, bone conduction hearing aid devices for single-sided deafness, as prosthetic devices under the Medicare benefit. Academy Advocacy Efforts In response to the proposed rule, Academy leadership and health policy staff advocated on multiple levels and engaged Academy committees, sister specialty societies and other leaders among our membership (within Otology/Neurotology as well as health policy and government affairs staff) to craft comments that best represent our members and our patients. More specifically, Academy leadership and staff conferenced individually and collectively with members and chairs of the Hearing and Implantable Hearing Devices Committees to gather specific examples and feedback on how the proposed rule, if enacted, would negatively impact thousands of patients who have no other recourse to better hearing. Further, the Academy participated in three direct meetings with CMS, various audiology and public interest group conferences, and meetings with presidents of ANS and AOS. All of these efforts were directed at raising awareness of the dangers of this proposed rule and garnering support in defense of our position. On September 2, 2014, the Academy, AOS, and ANS submitted a formal joint comment letter to CMS noting concerns about the proposal and providing a suggested alternative to the proposed rule that would allow for continued coverage of osseointegrated implants for Medicare patients. Our efforts will extend beyond the comment period as opportunities to positively influence any adverse CMS decision become evident. We will continue to closely monitor the matter and will be sure to keep members apprised of pertinent information via the eNews, HP Update, website, and other outreach tools. Members are encouraged to regularly check the Get Involved Regulatory Advocacy page for important announcements and opportunities to positively effect change. The Regulatory Advocacy page is at http://www.entnet.org/content/regulatory-advocacy. For the Academy leaders and members that took time out of your offices on short notice, or interrupted your vacations to personally participate in the aforementioned meetings and conferences, thank you. We greatly appreciate your dedication and willingness to get involved with these important policies.
Background
On July 11, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule focusing on payment policy updates to the 2015 Durable Medical Equipment, Orthotics, Prosthetics and Supplies (DMEPOS) fee schedule. Notably, as part of the rule, CMS is proposing to clarify the scope of the Medicare coverage exclusion for hearing aids and withdraw coverage of all types of air conduction and bone conduction auditory prosthetics (external, internal, or implanted). If finalized, the proposed rule would negate CMS’current coverage of osseointegrated implants.
CMS had expanded coverage to include osseointegrated implants as recently as 2005. In 2005, the auditory osseointegrated device was determined to be a new device category according to the new requirements for transitional pass-through payment during CMS’rulemaking. In the same regulatory revision, CMS additionally expanded coverage to both auditory osseointegrated devices and auditory brainstem devices, classifying them as prosthetic devices.
In the past, CMS has traditionally addressed the scope of the Medicare hearing aid coverage exclusion through program instructions and national coverage policies or determinations. However, this year, CMS decided to clarify the definition and its coverage determination of a hearing aid in its proposed rulemaking and comment period for DMEPOS payment rates.
CMS’ Rationale for its Proposed Coverage Exclusion
In the proposed rule, CMS states that bone conduction auditory prosthetics (along with other devices classified as “hearing aids”) do not meet the statutory definition of a prosthetic device found at section 1861(s)(8) of the Social Security Act which, in part, states a “prosthetic devices (other than dental) which replace all or part of an internal body organ.”CMS also states that osseointegrated implants are, “bone conduction hearing aids that mechanically stimulate the cochlea; therefore, we believe that the hearing aid exclusion applies to these devices and propose that Medicare should not cover these devices, consistent with our interpretation of section 1862(a)(7) of the Act.”CMS additionally mentions in the rule that a National Coverage Determination (NCD) was issued for cochlear implant devices with, “…the result that this determination and recent requests to expand coverage of hearing devices raises serious questions about the intent and scope of the Medicare coverage exclusion for hearing aids.”CMS also claims it initiated its examination of its definition of a hearing aid after receiving multiple benefit category determination requests in recent years for the consideration of non-implanted, bone conduction hearing aid devices for single-sided deafness, as prosthetic devices under the Medicare benefit.
Academy Advocacy Efforts
In response to the proposed rule, Academy leadership and health policy staff advocated on multiple levels and engaged Academy committees, sister specialty societies and other leaders among our membership (within Otology/Neurotology as well as health policy and government affairs staff) to craft comments that best represent our members and our patients. More specifically, Academy leadership and staff conferenced individually and collectively with members and chairs of the Hearing and Implantable Hearing Devices Committees to gather specific examples and feedback on how the proposed rule, if enacted, would negatively impact thousands of patients who have no other recourse to better hearing. Further, the Academy participated in three direct meetings with CMS, various audiology and public interest group conferences, and meetings with presidents of ANS and AOS. All of these efforts were directed at raising awareness of the dangers of this proposed rule and garnering support in defense of our position.
On September 2, 2014, the Academy, AOS, and ANS submitted a formal joint comment letter to CMS noting concerns about the proposal and providing a suggested alternative to the proposed rule that would allow for continued coverage of osseointegrated implants for Medicare patients.
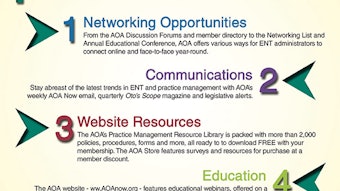
Our efforts will extend beyond the comment period as opportunities to positively influence any adverse CMS decision become evident. We will continue to closely monitor the matter and will be sure to keep members apprised of pertinent information via the eNews, HP Update, website, and other outreach tools. Members are encouraged to regularly check the Get Involved Regulatory Advocacy page for important announcements and opportunities to positively effect change. The Regulatory Advocacy page is at http://www.entnet.org/content/regulatory-advocacy.