Are You SURE It's Not My Sinuses?
From the Complementary/Integrative Medicine Committee, this article focuses on complementary treatments for headache, specifically migraine, which may be of assistance in treating patients.
William C. Hofmann, MD, and Scott R. Schaffer, MD, Complementary/Integrative Medicine Committee members

Causes of Facial Pain/Headache
It has been estimated that headaches are a problem for up to 50% of the world’s population, with migraine accounting for some 30% of headaches in adults from ages 16 to 65.1 A review published in 2020 estimated costs of migraine treatment alone is around $78 billion.2 Sinusitis and its related complaints account for over $2 billion in healthcare spending, with about 14% of adults reporting symptoms.3 It stands to reason that accurate diagnosis may decrease costs and improve patients’ lives.
A 2005 paper published in Otolaryngology-Head and Neck Surgery showed migraine disorders, not sinusitis, were responsible for facial pain and pressure in many patients; as to diagnosis, “The burden of diagnosing those migraine patients who present with pain primarily in the maxillary division of the trigeminal nerve, often with rhinitic symptoms, will likely fall on otolaryngologists.” 4 Should normal due diligence show no significant evidence of sinusitis or other causes for headache, migraine should be considered.
It is also common for many patients to seek other solutions to their discomfort, perhaps non-medicinal. It has been estimated that around 50% of patients will try complementary and/or integrative treatments for their issues.5 This article will focus on complementary treatments for headache, specifically migraine, which may be of assistance in treating patients.
A formal diagnosis of migraine can be made after meeting certain criteria. A patient must have had five episodes of headache or pain lasting anywhere from 4 to 72 hours. Pain must be accompanied by nausea and vomiting, or the patient must experience photo- or phonophobia. These cannot be caused by another disorder. In addition, the patient must have at least two of the following signs: unilateral pain, pulsating quality, pain of moderate or severe intensity, enough discomfort to affect daily activities, or aggravation of pain with routine activity.6 In the past, this was thought to be due to vascular problems but has more recently been attributed to a neurovascular issue, with sensitization of trigeminal fibers affecting the blood vessels and meninges they innervate. The initial event seems to be a hyperexcitability of the nerve fibers.7 Rhinitic symptoms including congestion and nasal drainage may occur due to stimulation of the parasympathetic system involving connections from the trigeminal nerve to the facial nerve via the superior salivatory nucleus. These rhinitic symptoms are what make the patient feel that their problem is due to a sinus issue rather than migraine, since such symptoms are not part of the International Headache Society classification system.4
Rhinitic and autonomic signs are also seen in cluster headache, but this form of headache is marked mostly by its severity and pattern of attack. It is most often seen in men, is unilateral, and can be excruciating. Fortunately, this form of headache is quite rare, affecting about 0.1% of the population. Unlike migraine, patients with cluster headache tend to be restless and have been known to hit their head against a wall to distract from the pain. Like the pain, rhinogenic and autonomic signs are unilateral only. The headache may have a genetic component, passing in autosomal dominant fashion. For those with a first-degree relative, the risk of cluster headache can be 5 to 15 times greater than the general population. Attacks tend to take place over weeks to months and then may go into remission for years at a time. Triptans can be effective in treatment, as can oxygen at high flow. Calcium channel blockers are also very effective in terms of treatment.8,9
Temporomandibular joint disorders are a common issue that can lead to headache. It can affect up to 15% of adults, most commonly from ages 20 to 40. It is much more common in women than in men. Patients may note severe pain with jaw movement, as well as pain on awakening. Interestingly, few patients require treatment, as it can resolve spontaneously in about 40% of those afflicted. However, pain can be quite severe. For those patients, therapy including bite splints, medications, and cognitive therapy can be of help.10
Post-traumatic headache is one of the more disabling sequelae of a concussion and can mimic migraine in terms of severity. Several possible pathophysiologies have been proposed, including activation of the trigeminovascular system as is seen in migraine. Thus far, treatment has followed guidelines for tension headache as well as migraine, including use of complementary therapies for chronic sufferers.11,12
Facial pain/headache can also be caused by true sinus infection. This is frequently viral, but chronic bacterial sinusitis can develop after prolonged inflammation and impairment of normal mucociliary flow out of the sinuses.
Dietary and Lifestyle Factors
Headache patients sometimes note that specific foods or beverages lead to a severe headache. The number of patients reporting triggers tends to vary widely, ranging from 10% to 64% of patients in a review of studies. Commonly reported triggers include chocolate, alcohol, and nitrates in preserved meats. However, studies examining the link between food triggers and onset of migraine often do not show a link. Moreover, individuals reporting a specific trigger often find that trigger will not reliably induce a migraine.13 Because of this, discovery and avoidance of triggers can be exceptionally difficult.14
Other studies have focused on the quality of diet as a predisposition to migraine. For example, Hajjarzadeh, et al. noted that women who consumed a Western diet, high in processed foods, sugar, and salt, had a higher frequency of migraine as opposed to those partaking of a healthier diet consisting of vegetables, fruits, and legumes.15 Another review showed following a low lipid diet induced fewer migraines than a high lipid diet. High body mass index was also associated with an increased risk of migraine. The authors noted that most studies reviewed were of low quality, often not comparing findings with studies evaluating standard pharmacologic therapy.16
There are some steps patients may take to determine patterns to their headaches and to see if there are triggers to avoid. Keeping a headache journal can be very helpful, as it can allow for pattern recognition. Although the influence of diet is not certain, it is advisable to follow a healthy lifestyle of exercise, adequate rest, hydration, and healthy diet. This may be the most beneficial intervention as opposed to trying to avoid triggers. Fear of migraine, or cephalophobia, should be recognized and treated aggressively, as stress has been linked to migraine frequency. A cognitive approach is often the best way to address this.15
Treatment
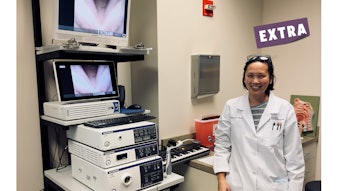
One of the most important aspects of treatment is patient education and acceptance. In our experience, this can be the most difficult part of the process, as patients often have a preconceived idea of what constitutes a migraine. A thorough evaluation, including endoscopy and even computed tomography exams, can be very helpful in allowing patients to understand that sinus issues are not the cause of their problems and that a different approach can be effective in controlling their symptoms.
Use of vitamins and minerals for prevention of migraine is a common practice, especially for those who suffer from a more chronic form. Levels of evidence are variable, however, and studies reviewed suggest further investigation is needed.
Magnesium supplementation has been evaluated in the past by the American Neurological Association (ANA) and has shown to be moderately effective for treatment. It is thought to act by reducing cortical hyperexcitability, most likely by blocking calcium channels. Its use has shown a higher efficacy at preventing an attack than placebo. Although its use is generally safe, it should be avoided in patients with renal failure.17,5
Use of B-complex vitamins, predominantly riboflavin (B2), has also been evaluated by the ANA and is thought to act by affecting mitochondrial dysfunction, thereby reducing cortical activation. Like magnesium supplementation, it has been thought to be moderately effective. Coenzyme Q10 is a newer addition that seems to act as an antioxidant, thereby reducing inflammation.5,18
A variety of integrative and wellness therapies have been evaluated. Quality of evidence tends to be low-to-moderate over these studies, and again, further evaluation and study are needed. Therapies studied include acupuncture, directed meditation, yoga, and biofeedback.18 The importance of a healthy lifestyle should be emphasized, including use of regular aerobic exercise. Although not a stand-alone treatment, it has been recommended for use as a preventive strategy to control migraine.5 Transcranial magnetic stimulation (TMS) has been shown to reduce headache in a high percentage of migraine sufferers.19
It should also be noted that these therapies and interventions may not be covered by insurance, making them an out-of-pocket expense for many patients.
Summary
Facial pain and pressure, often thought by patients to be caused by bacterial sinusitis, are more often a form of migraine and can respond to migraine treatment. Patients may find this difficult to accept. A thorough evaluation and calm education are key for patient recognition. A variety of non-medicinal therapies can be offered, and some, including healthy diet, adequate rest, hydration, and aerobic exercise, can be very beneficial.
References
- Stovner LJ, Hagen K, Linde M, et al. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain 2022;23(1):34. doi: 10.1186/s10194-022-01402-2
- Polson M, Williams T, Speider L, Mwamburi M, Staats P, Tenaglia A. Concommitant medical conditions and total cost of care in patients with migraine: a real-world analysis. Am J Manag Care. 2020;26(11):53-57.
- Battisti AS, Modi P, Pangia J. Sinusitis. Sinusitis. StatPearls. Published January 2022. Updated August 8, 2022. https://www.ncbi.nlm.nih.gov/books/NBK470383/
- Mehle M, Schreiber C. Sinus headache, migraine, and the otolaryngologist. Otolaryngol. Head Neck Surg. 2005;133(4):489-496. doi: 10.1016/j.otohns.2005.05.659
- Patel P, Minen M. Complementary and integrative health treatments for migraine. J Neuroophthalmol. 2019;39(3):360-369. doi: 10.1097/WNO.0000000000000841
- Mongini F. Migraine. In: Headache and Facial Pain. 1st ed. Thieme; 1999:189-202.
- Welch K. Contemporary concepts of migraine pathogenesis. Neurology 2003;61(suppl 4): S2-S8. doi: 10.1212/wnl.61.8_suppl_4.s2
- Kandel SA, Mandiga P. Cluster headache. StatPearls. Published January 2022. Updated July 18, 2022. https://www.ncbi.nlm.nih.gov/books/NBK544241/
- Vollesen A, Benemei S, Cortese F, et al. Migraine and the cluster headache-the common link. J. Headache Pain. 2018;19:89-104. doi: 10.1186/s10194-018-0909-4
- Gauer R, Semidey M. Diagnosis and treatment of temporomandibular disorders. Am Fam Physician 2015;91(6):378-386.
- Ashina H, Porreca F, Anderson T, Amin F, Ashina M, Schytz H, Dodick D. (2019) Post-traumatic headache: Epidemiology and pathophysiologic insights. Nat. Rev. Neurol. 15(9): 607-619.
- Kamins J. Models for Treating Post-traumatic Headache. Curr Pain Headache Rep. 2021 Jun 14;25(8):52. doi: 10.1007/s11916-021-00970-3. PMID: 34125320; PMCID: PMC8203551.
- Zaeem Z, Zhou L, Dilli E. Headaches: a review of the role of dietary factors. Curr Neurol Neurosci 2016;16:101-112.
- Marmura M. Triggers, protectors, and predictors in episodic migraine. Curr Pain Headache Rep 2018;22(12):81-90. doi: 10.1007/s11916-018-0734-0
- Hajjarzadeh S, Mahdavi R, Shalilahmadi D, Nikniaz Z. The association of dietary patterns with migraine attack frequency in migrainous women. Nutrit Neurosci. 2020;23(9):724-730.
- Rehman T, Ahmad S, Fatima Q. Effects of dietary supplementations and herbs on migraine-a systematic review. J Comp Integrat Med. 2019;16(3):1-11.
- Domitrz I, Cegielska J. Magnesium as an important factor in the pathogenesis and treatment of migraine-from theory to practice. Nutrients. 2022;14:1089-1101.
- Millstine D,Chen C, Bauer B. Complementary and integrative medicine in the management of headache. BMJ. 2017;357:j1805.
- Bhola R, Kinsella E, Giffin N, et al. Single-pulse transcranial magnetic stimulation (sTMS) for the acute treatment of migraine: evaluation of outcome data for the UK post market pilot program. J Headache Pain 2015;16:51 . doi: 10.1186/s10194-015-0535-3