Crossing the payment bridge
On April 27, 2016, the Centers for Medicare & Medicaid Services (CMS) released the long-awaited replacement for the Sustainable Growth Rate (SGR) as the payment system for physicians participating in Medicare: the Merit-based Incentive Payment System (MIPS) and Alternative Payment Model (APM) programs.
Long-awaited post-SGR payment is here

Merit-based Incentive Payment System
Under the new MIPS program, starting January 1, 2017, physicians will report on four categories that add up to a composite score, which CMS will use to determine whether or not Eligible Clinicians (ECs), including most otolaryngologist-head and neck surgeons, receive a bonus payment or are subject to a payment reduction for 2019 payments. The graphic at right, courtesy of CMS, provides a broad explanation of the four categories ECs will begin reporting in 2017.
Alternative Payment Models
ECs may be exempted from the MIPS program if they participate in a CMS-defined Advanced APM. An Advanced APM requires participants to use certified EHR technology; provide payment for covered professional services based on quality measures comparable to those used in the quality performance category of MIPS; and be either an expanded Medical Home Model or bear more than a nominal amount of risk for monetary losses. The Academy expects otolaryngologist-head and neck surgeon participation in Advanced APMs to be low due to the strict eligibility criteria.
Some ECs may participate in a MIPS APM to receive bonus points and alternative scoring criteria for the MIPS program. MIPS APMs are participants of CMS-defined APMs, such as a Track 1 Accountable Care Organization, that do not meet Advanced APM criteria.
For a more detailed outline and further explanation of the reporting criteria for the MIPS and APM programs, please see the Academy’s summary on page 22. Members can also access more detailed information on the MIPS and APM programs at www.entnet.org/content/physician-payment-reform.
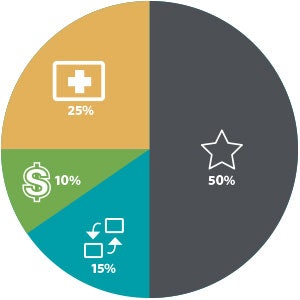
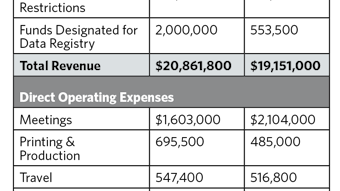
COST10 percent of total score in year 1; replaces the cost component of the Value Modifer Program, also known as Resource Use
The score would be based on Medicare claims, meaning no reporting requirements for clinicians. This category would use more than 40 episode-specific measures to account for differences among specialties.
QUALITY
50 percent of total score in year 1; replaces the Physician Quality Reporting System and the quality component of the Value Modifer Program
Clinicians would choose to report six measures versus the nine measures currently required under the Physician Quality Reporting System. This category gives clinicians reporting options to choose from to accommodate differences in specialty and practice.
CLINICAL PRACTICE IMPROVEMENT ACTIVITIES
15 percent of total score in year 1
Clinicians would be rewarded for clinical practice improvement activities focused on care coordination, beneficiary engagement, and patient safety. Clinicians may select activities to match their practice goals from a list of more than 90 options. In addition, clinicians would receive credit in this category for participating in Alternative Payment Models and in Patient-Centered Medical Homes.
ADVANCING CARE INFORMATION
25 percent of total score in year 1; replaces the Medicare EHR Incentive Program for
physicians, previously known as “Meaningful Use”
Clinicians would choose to report customizable measures that reflect how they use electronic health record (EHR) technology in their day-to-day practice, with a particular emphasis on interoperability and information exchange. Unlike the existing Meaningful Use program, this category would not require all-or-nothing EHR measurement or quality reporting.